Covid: Care home deaths 'like losing family', say staff
- Published

A year on from the peak in coronavirus deaths among care home residents in England and Wales, there are increasing calls for a public inquiry.
Many in the sector believe the government ignored their plight until the death toll made that impossible to do.
Twelve months ago, nursing associate Damian Mann was desperately trying to save the lives of people he spends more time with than his relatives, every day.
Damian works at Wren Hall Nursing home in Nottinghamshire, and between the end of March and mid-April 2020, 13 residents died with Covid-19.
"Some of the people have lived here for five, six years. I see them more than my own family.
"And then they're not here any more," he remembers.
Damian was working on the hastily set-up isolation unit. He was one of just a few staff who didn't contract the virus, so saw resident after resident pass away.
"We would always make sure someone was with them," he says.
"You thought to yourself, if I emotionally connect with every scenario… you're going to have a breakdown, because you're not going to be able to get yourself right."
The residents who died were like family, says nursing associate Damian Mann
At the time, most of the government's and the country's attention was focused on preventing the NHS being overwhelmed, but in the first weeks of April the number of residents dying in care homes was rising rapidly.
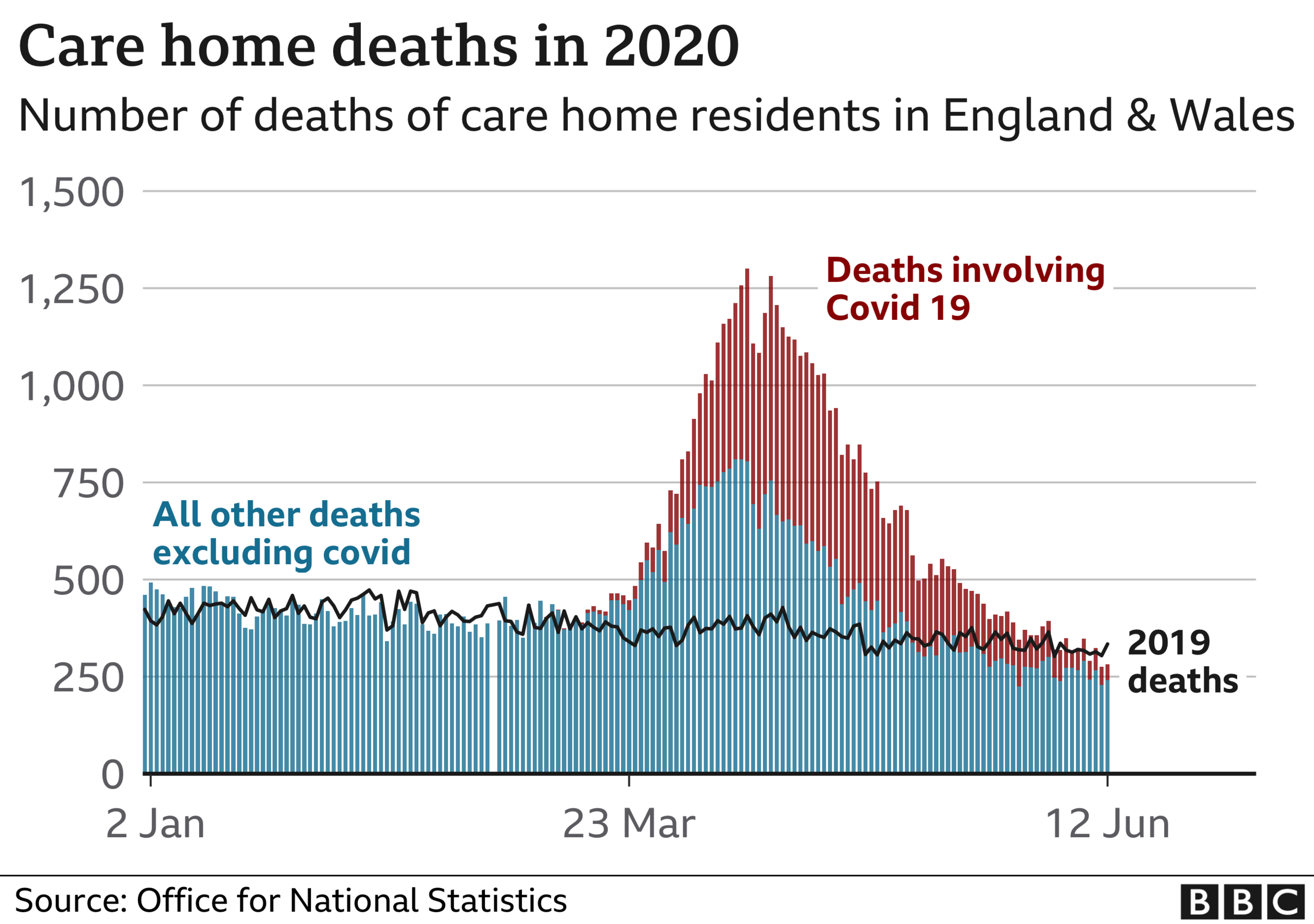
Easter Sunday, 12 April 2020, saw the highest number of care home deaths during the pandemic in England and Wales, according to the Office for National Statistics: , external
1,300 residents died, nearly three times the number who died on the same day in 2019
495 of these died with Covid
On each of the 20 days from 5 April:
there were more than 1,000 deaths of care home residents from all causes, double the expected level
of these, the numbers whose death certificates mentioned coronavirus peaked at 540 on 17 April
Patients were being rapidly discharged from hospitals to care homes without being tested, agency staff could move between homes, there was little testing available and some care homes struggled to get sufficient medical support.
'Feeling numb'
Damian remembers that, initially, the guidance said PPE should be changed every time a staff member assisted a resident but "within two weeks it changed so you could then help three individuals and then change your PPE. You were thinking it doesn't seem right and feel comfortable to be doing this."
A government spokesperson told the BBC it had done "everything possible" to protect care homes.

On social media, care home owner Anita Astle described the situation as dire
Anita Astle owns Wren Hall, and last spring she was desperate to alert people to what was happening.
On 31 March, on social media, she described the situation as dire.
On 12 April she tweeted:, external "Feeling numb - lost nine family members (residents) in last few days."
She says the government guidance was atrocious and believes social care was overlooked at the start.
"We were clapping for the NHS, we were hearing 'protect our NHS', but there was nothing about social care. It's probably a sad state of affairs that I don't feel angry. I just feel that's the norm."
Through glass
The same day Anita posted her tweet, Jean Adamson was trying to see her father through the window at his care home in London. He had Covid.
She describes Aldrick Adamson, who was part of the Windrush generation, as fiercely independent, a family man and a musician.
That day, on the other side of the glass, he was singing to himself, but Jean says he knew she was there.

Aldrick Adamson, 98, died on 15 April last year
It was the last time she saw him.
"He just went downhill so quickly," says Jean.
"I still need to know why my father died in a place where he was supposed to be safe from harm.

Jean Adamson is part of a group of families campaigning for a public inquiry.
"The government has a legal and moral responsibility to get to the truth, so that people who are bereaved like myself, get the answers and can grieve and get closure, and also, to save people's lives in the future."
On 15 April, the day Aldrick died and as the virus was at its peak in care homes, the government published its social care plan.
'Badge of honour'
Health and Social Care Secretary Matt Hancock told a Downing Street press conference: "From the moment of the emergence of coronavirus, we've known that some of the most vulnerable to this disease are in social care, and we've been taking action right from the start."
He announced that patients being discharged from hospitals into care homes would all now be tested.
Testing was also extended for care staff and symptomatic residents, more PPE was promised and he gave his backing to a "badge of honour" for care workers.
Back at Wren Hall, when David Capewell remembers last April tears begin to roll down his cheeks.
His wife, Anthea, was one of the residents who contracted the virus.

David Capewell greets his wife Anthea through a care home window
He got a call from the home saying she might not last through the night: "One of the nurses said 'you had better come in quick'. Anthea didn't look well at all. I spent most of the night with her."
Anthea survived. With restrictions on visiting, David had been able to see very little of her, so he now volunteers as a gardener at the home.
It means when he has a break, he can sit on the other side of her window, allowing them to spend extra time together.
"It's such a relief, just to see her through the window," he says.
"This thing, I hope it goes away so quickly. And that we can all get back to some sort of normality."
'Human tragedy'
A government spokesperson responded: "Every death from this virus is a human tragedy and our heartfelt sympathies go out to everyone who has lost a loved one.
"From the start of this global pandemic we have done everything possible to protect care homes, including placing residents and staff in the highest priority group for vaccinations.
"We have increased staff testing to identify new cases and protect residents, while providing almost £1.8bn in specific funding for adult social care and access to over £6bn for local authorities to address pressures on public services, including free PPE for adult social care.
"Our vaccination programme is the biggest in NHS history, and through the rollout we have visited every eligible care home in England, offering lifesaving vaccines to all residents and staff."