GPs say shortage of doctors puts safe care at risk
- Published

Prof Martin Marshall says GP workloads mean they are more likely to make a mistake which could harm patients
GPs in England are finding it "increasingly hard to guarantee safe care" as the number of doctors falls and demand surges, a senior medic said.
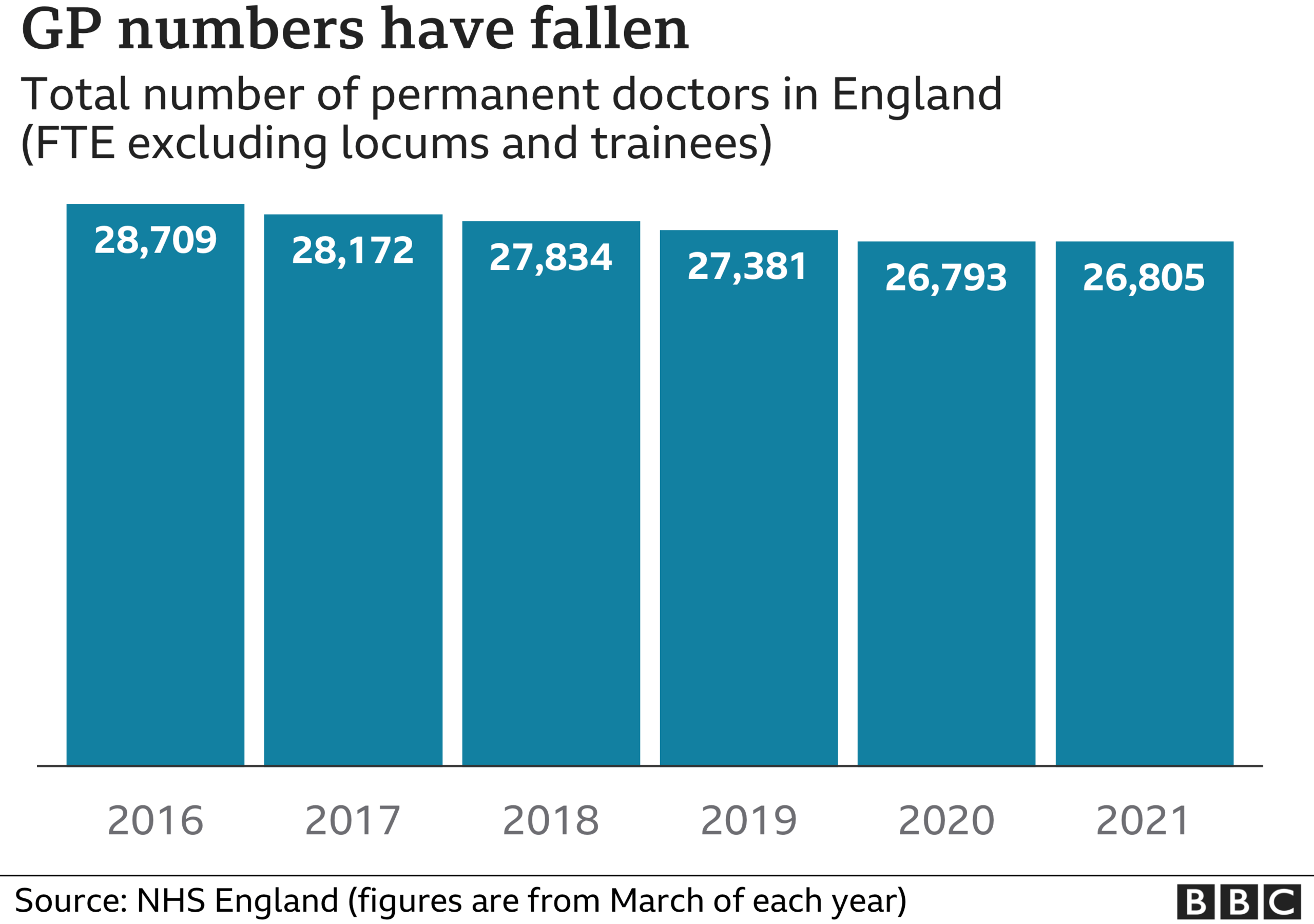
Prof Martin Marshall, chair of the Royal College of GPs, told the Guardian, external GP numbers had fallen by 4.5% despite an ageing population with an increased need for care.
GPs feared making serious mistakes due to excessive workloads, he said.
Prof Marshall also defended the continued use of remote consultations.
In 2015, the government promised to hire 5,000 extra GPs within five years, but instead the Royal College of GPs says between September 2020 and March 2021 numbers fell by 1,307 to 28,096.
At the 2019 election, then Health Secretary Matt Hancock admitted they had failed to meet the recruitment target, as the Conservatives made a fresh promise to recruit 6,000 more GPs by 2025.
Prof Marshall said the demand for services from GPs, including more complex consultations and the vaccination programme, on top of this decline in numbers was putting family doctors under strain.
"The fact that general practice is under such enormous pressure means it can't deliver the patient-centred services that it wants to. Many GPs are even finding it challenging to maintain a safe service," he said.
He said family doctors were more likely to make a mistake if they were working 11- or 12-hour days, seeing 50 or 60 patients.
"GPs are finding it increasingly hard to guarantee safe care to their patients," he said. "The chances of making a mistake in a diagnosis or a mistake in a referral decision or a mistake in prescribing are all greater when you're under stress."

Prof Marshall spoke as GPs faced criticism over the continuing difficulty for some patients in accessing face-to-face appointments.
Health Service Journal reported that one coroner had raised remote consultations as a risk, external during the inquests into five separate deaths.
Prof Marshall said remote appointments had been necessary during the pandemic to keep staff safe and avoid spreading the virus.
He said many patients welcomed them as more convenient. But while he said patients who "absolutely need" face-to-face appointments for clinical reasons are given them, GPs were "struggling" to meet demand from patients who would prefer in-person consultations.
The RCGP is calling for an emergency rescue package to support surgeries, including recruiting 6,000 more GPs and 26,000 support staff such as nurses and receptionists by 2024.
On Tuesday, the prime minister announced a new health and social care levy, which is intended to provide extra funding to ease pressure on the NHS over the next three years.
Related topics
- Published8 September 2021

- Published27 May 2021

- Published14 July 2021
