Jasper Brooks inquest: Baby died due to 'neglect' at hospital
- Published
A coroner has found neglect contributed to a baby's death at the hospital where he was born.
Jasper Brooks died at the Darent Valley Hospital in Kent on 15 April 2021.
The coroner found gross failures by midwives and consultants at the hospital and says Jasper's death was "wholly avoidable".
The Dartford and Gravesham NHS Trust says: "We are committed to learning from our mistakes to ensure no family has to go through this again."
It added: "We are very sorry for the devastating impact this has had on the Brooks family.
"We have already taken significant action to improve our practices and will commit to implementing the additional recommendation from the inquest."
Jasper was a second child for Jim and Phoebe Brooks. Their first, Oscar, had also been born at the Darent Valley Hospital.
On that occasion, the family had received good, prompt care after Phoebe had suffered a placental abruption - a serious condition in which the placenta starts to come away from the inside of the womb wall.
That complication was the reason Phoebe was booked in to have an elective Caesarean section to deliver Jasper. But in April 2021 those plans changed overnight.
A check-up found Phoebe had raised blood pressure. She was told to remain in hospital and that the C-section would happen the following morning - nine days earlier than planned - when there were more staff on duty.

Phoebe and Jim Brooks - Jim says there is a taboo when talking about baby loss
Jasper's parents say the midwives caring for Phoebe repeatedly failed to listen to her and Jim's concerns - that she was shaking violently, feeling sick, and thought she was bleeding internally.
"We felt like an inconvenience - no-one wanted to deal with me that night," Phoebe says. "The doctor didn't want to do my C-section, the midwife that's meant to be looking after me, she just doesn't really care.
"I remember saying clearly to her, 'my whole body is shaking - something's happening, and no-one's taking the time to listen to what I'm saying or listen in on my baby'."
Phoebe went into labour naturally, before the C-section could take place.
At the inquest hearing, midwife Jennifer Davis was accused by the family's barrister, Richard Baker KC, of "failing to act on signs of blood loss, failing to determine if Phoebe was in active labour, and failing to call a senior doctor when necessary".
Ms Davis told the inquest that she had been traumatised by the case.
"I thought, on the night, I was giving the best care I could," she said. "Everything I did that night wasn't done with any intent to harm."
Prior to baby Jasper's birth, staff struggled to find the unborn baby's heartbeat and did not spot that Phoebe was about to deliver.
"His whole body was born all at once," Phoebe says, "I looked down and he was just so white. And then all of a sudden it was like, panic. One of the midwives picked up the baby and started rubbing him and was like, 'come on baby, come on baby'.
"Then I thought, 'he's going to cry, he's going to cry. Why is baby not crying?'"

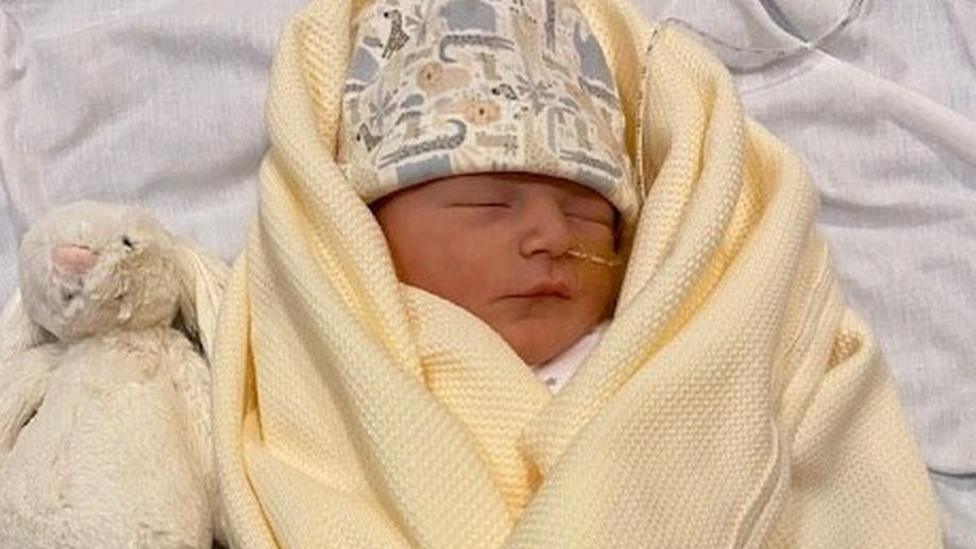
Phoebe holding baby Jasper
Jasper was born without a heartbeat, so a resuscitation team was called. But during the inquest, the family learned that further errors were made because the correct people failed to attend the resuscitation.
There was no consultant neonatologist on site - a doctor with expertise in looking after newborn infants or those born prematurely. Intubation, the process of placing a breathing tube into the windpipe - which should only take a few minutes - did not occur for 18 minutes. There was also a delay in administering adrenaline to try to stimulate Jasper's heart.
Twenty-seven minutes after Jasper was born, and with a heartbeat still not evident, a consultant told Jim and Phoebe they were going to stop working on their son.
"We were just in complete shock, 'how has this happened?'," says Phoebe. "I reached out and touched him, and basically his heartbeat came in, and then, all of a sudden, they were like, 'we've got a heartbeat'.
"They went from calling time - they're going to end life, and end resuscitation - to he's got a normal heartbeat."
The newborn was taken away for tests, but shortly afterwards a doctor returned and told the family further treatment would be futile because Jasper was very ill.
The family asked if he could be moved to another hospital for more specialised care - the possibility of which had already been mentioned - but were now told there would be no point.
National guidelines state the decision to end care should be made by a multidisciplinary team comprising at least two consultants - not just a single doctor, the family later learned.
"We did not agree with the plan they made," says Phoebe. "We asked if there's any other options, and we were told, 'no. You're going to go into monkey room [bereavement suite] and Jasper's going to die'.
"I remember holding him, uncontrollably crying, and just trying to treasure that moment with our son while we're waiting for him to die. But he kept taking another breath and another breath."
The longer Jasper lived, the more his parents were keen further treatment be offered. They were finally given permission to feed him when Jasper was 12 hours old.
Rather than dying within minutes, as his parents had been told he would, Jasper died on 15 April 2021, having lived for 23 hours.
"It was a complete shambles," says Jim, a director at a construction company. "He lived for a day," adds Phoebe, who works as a personal assistant.
"We wanted a lifetime with him, which was taken away from us because of how that hospital treated me in labour and how they treated him."
Inquiries into poor maternity care have already been held in Morecambe Bay, Shrewsbury and Telford, and East Kent, with a review ongoing in Nottingham.
But such are the concerns about care in many other units that some campaigners now argue that a national inquiry is needed, not reviews into individual trusts.

Jasper was born at Darent Valley Hospital in April 2021
Rhiannon Davies lost her daughter at the Shrewsbury and Telford Hospital Trust in 2009. Her complaints led to the Ockenden report on safety and standards - the largest inquiry of its kind in the history of the NHS.
"We still hear of the same mistakes being made - and often, they are basic errors, but they are catastrophic in terms of their impact," Ms Davies, who has written to the health secretary asking for a wider inquiry, says.
"It's fair to say what we've tried so far hasn't worked. Neither has increased investment and greater public awareness of maternity risk. We need a national inquiry resulting in national measures that can properly protect people from avoidable harm and death."
Since Jasper's death, Phoebe and Jim have had a daughter, Primrose, a sister for Oscar.
But when asked, they say they have three children, not two.
"He will always be part of the family," says Jim.
Related topics
- Published7 September 2023

- Published2 April 2022

- Published11 July 2019
