Mental health trusts restrain patients 'every 10 minutes'
- Published
Mental health trusts in England are restraining patients on average every 10 minutes, figures have revealed.
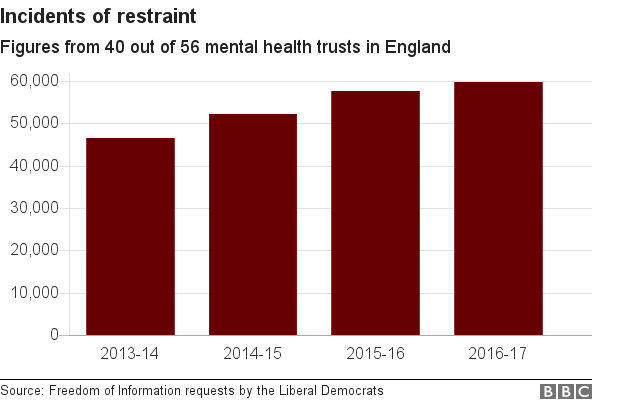
They show the number of incidents of restraint has increased each year since 2013.
Former health minister Norman Lamb said use of force was "endemic" in many units.
The Department of Health said it was working with the Care Quality Commission (CQC) to ensure the use of restraint is minimised.
Six restraints an hour
Figures from 40 mental health trusts in England revealed patients were restrained 59,808 times in 2016-17, equivalent to between six and seven incidents an hour.
This compares with 46,499 times in 2013-14.
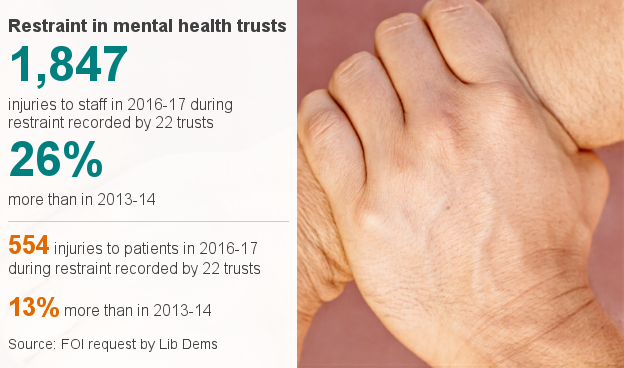
The figures, released to the Liberal Democrats under the Freedom of Information Act, also showed an increase in injuries to patients and staff
However, use of the most extreme restraints, where patients are forced to the ground, fell 9% across 33 trusts.
Mental health trusts say they have improved their reporting of their use of restraint, which may have contributed to some of the rise.
Physical restraint is classed as "any direct physical contact where the intention is to prevent, restrict, or subdue movement of the body (or part of the body) of another person".
The Department of Health, external says there must be "a real possibility of harm to the person or to staff, the public or others" for restraint to be used.

'Treated like an animal'

Liz Rotherham believes it was unnecessary to restrain her
Liz Rotherham suffers from psychotic episodes and said she has been restrained in hospital on three occasions.
She claimed it happened at the The Linden Centre in Chelmsford and The Lakes in Colchester. The most recent was in 2013.
"I don't know why they felt the need to it," said the 46-year-old from Essex. "I wasn't throwing things around, I wasn't being abusive or anything like that.
"They actually hurt me, which wasn't very nice. I had six people holding me down on a crash mat. They pulled down the side of my knickers and injected me."
She said that a female police officer attending the unit once told her "don't be a wuss".
"I will never, ever forget that. I felt like I was being treated like an animal."
Ms Rotherham said she believed someone could have sat down and talked to her without the need for restraint.
The Essex Partnership University NHS Foundation Trust, which runs the hospitals, said it could not comment on an individual patient's case.

'Concerning rise'
Dr Sridevi Kalidindi of the Royal College of Psychiatrists said the data showed some trusts were making progress but consistent improvements were not being seen across the board.
"The increase in the number of restraints recorded is concerning," she said. "Cuts to bed numbers and community care programmes mean you now have to be more ill to be admitted to a mental health unit."
Dr Kalidindi said increasing use of agency staff meant fewer permanent staff trained to de-escalate situations were available.
'Humiliating, terrifying'
Lib Dem health spokesman Norman Lamb said: "Many inspiring units have demonstrated how you can very significantly reduce the use of force, training staff in de-escalation.
"This can avoid situations which lead to stress and conflict. This needs to be given much greater priority by the Government."
Vicki Nash of mental health charity Mind, said: "Physical restraint can be humiliating, terrifying, dangerous and even life-threatening.
"There is currently a Private Members' Bill going through parliament which, if it becomes law, has the opportunity to increase transparency and accountability around the use of force in mental health settings."
A Department of Health spokeswoman said: "Physical restraint should only be used as a last resort and our guidance to the NHS is clear on this.
"We want patients to be treated and cared for in a safe environment and we are actively working with the regulator, the Care Quality Commission, to ensure the use of restraint is minimised."
- Published22 September 2017

- Published25 April 2017

- Published3 August 2017

- Published21 September 2016
