Sickle cell: 'Blood transfusions have saved my life many times'
- Published

Sadeh Graham requires regular transfusions to manage her sickle cell
About 800 blood donors with black heritage are needed in the West Midlands as demand for sickle cell treatment increases.
The NHS reported a 60% increase in demand from hospitals in the region and anticipates that to rise further.
It said the biggest demand was in Birmingham and appealed for more people to sign up to donate their blood.
Sickle cell causes red blood cells to form into crescent shapes which can cause fatal complications.
The disease is particularly common in people with an African or Caribbean family background and many patients need regular transfusions to stay alive.
Sadeh Graham, 29, from West Bromwich, needs all her blood replaced by donor blood every four weeks.
"Some days I struggle to get out of bed and have a shower due to the sheer pain in my limbs," she said.
"Some days I wake up feeling great, and some days I wake up in hospital, connected to machines and told that days have passed."

What is sickle cell disease?
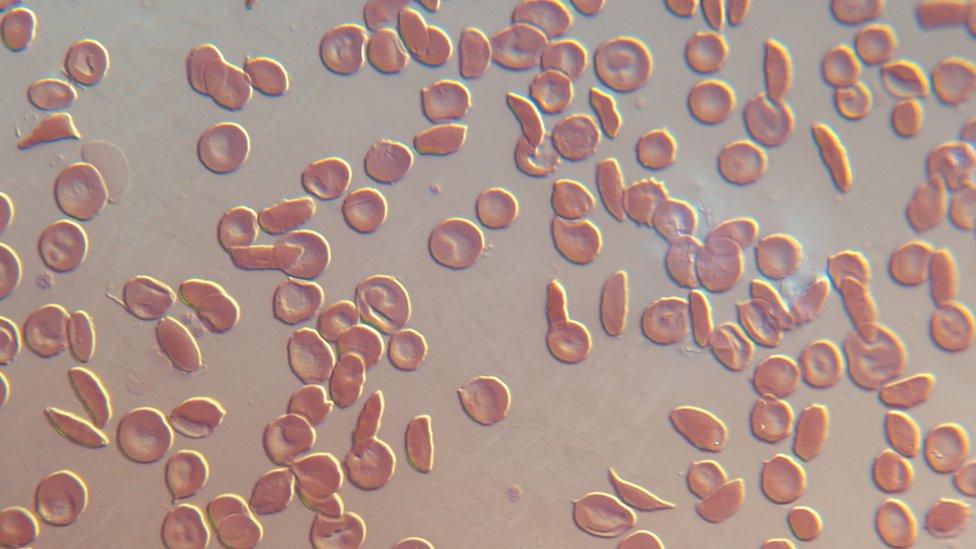
People with sickle cell disease produce unusually shaped red blood cells
Sickle cell disease is the name for a group of inherited health conditions that affect red blood cells.
People with sickle cell disease, external produce unusually shaped red blood cells that can cause problems as they do not live as long as healthy cells and can block blood vessels.
It is particularly common in people with an African or Caribbean family background.
Sickle cell disease is a serious and lifelong health condition, although treatment can help manage symptoms, which can include anaemia, lung problems and strokes.
Source - NHS, external

Transfusions help with her energy levels, meaning Ms Graham is able to work and socialise.
"Blood exchange transfusions have saved my life many times over," she said.
"After each transfusion, I feel like a new and improved version of myself."
The NHS said it currently was only able to match patients' blood types in just over half of requests and in many cases had to rely on using O-negative, which is a universal blood type.
"Matched blood is vital for sickle cell patients to reduce the risk of serious complications," said consultant haematologist Dr Rekha Anand.
"People from the same ethnic background are more likely to have matching blood. We urgently need more black people in the West Midlands to become regular donors."

Follow BBC West Midlands on Facebook, external, Twitter, external and Instagram, external. Send your story ideas to: newsonline.westmidlands@bbc.co.uk
Related topics
- Published4 October 2022

- Published13 June 2022

- Published24 February 2022
