Family members worry as eating disorder support service stopped
- Published

Tia has daily video calls with a nurse
A one-to-one-video call service that was brought in during lockdown to support people with eating disorders is being stopped. One person has said the service saved her partner's life, while a 19-year-old has said she is now worried for the future.
Funded through the Avon and Wiltshire Mental Health Partnership (AWP), the trust said that it was only ever meant to be temporary and they are bringing in new services which will provide improved care.
Tia is sat in the kitchen with a laptop set up in front of her.
She is on a daily call with her nurse who is counting her down from five to one.
At one, Tia pulls back the lid on a rice pudding.
The nurse reassures 19-year-old Tia, from Yate, and encourages her to eat.
Tia has been receiving these calls for around a year, but at the end of March, the Eating Disorder Home Care (EDHC) service is due to stop.
Warning: This article contains an image some readers might find upsetting

Tia said she was bullied when she was younger
Three years ago, Tia was studying at school and playing rugby, but she said she was bullied for being "bigger" and had body image issues.
When lockdown came in March 2020 she decided she wanted to come out of it "brand new".
She lost a lot of weight and people complimented her on her new look, but before long it "spiralled out of control," she said.
Tia's brain and body were massively undernourished. She was cold all the time, losing her hair, bruising easily and could not sleep properly.
In 18 months she said she lost half her body weight.
Tia was in and out of hospital "so many times I lost count" and there were serious concerns about her heart, which had shrunk in size.

Tia lost half her body weight
Tia spent days hooked up to hospital machines. "They were really dark days - we were told she was dying," mum Jo said.
Jo was contacted about the EDHC service, which she was keen to take up, and Tia was sent home under their care.
"I am so thankful that they came to my mum and asked my mum, because I know I may not have taken it up... it has changed my whole life," Tia said.
"They have got me through so many hard moments... and have been there every step of the way."
Video calls would take place up to six times a day, during which a specialist would guide patients through eating snacks and meals.
Without them, Tia said she just would not eat.
"I just can't do it by myself. I really struggle and that is something me and my therapist are still working on," she said.

Tia's mum Jo is concerned there "is no plan in place" for when the service ends
Tia's family said the service has kept her out of hospital - with the nearest available inpatient space being in Manchester. It also allows her to be supported at work and while on holiday.
Jo added: "I genuinely don't know what we would have done without them.
"The opportunity for her to be able to stay at home, us stay as a family... was everything really.
"There were so many days that we would have ended up at A&E because we were exasperated.
"We couldn't do it by ourselves. It has given us our life back."
Now EDHC is ending, Jo said she is worried about what the future may look like.
"I'm really worried that there doesn't seem to be a plan in place," she said.
"We've not had a conversation at all and it is only next month."

Tia said she has been improving since receiving support from EDHC
The service was set up in the winter of 2021 and had 43 referrals, although only about half stuck with the programme.
Currently, it has about nine people using the service ahead of its closure in March.
AWP said the temporary service was brought into Bristol, North Somerset and South Gloucestershire (BNSSG) at a specific time, to deal with specific problems - including a shortage of staff, a lack of inpatient beds and the fact lockdown meant they were unable to visit patients in person.
It added that while it is pleased the calls have been helpful to some, it also risks creating dependency rather than treating the causes of the eating disorder.
AWP said it has now increased its eating disorder team staff from 10 to 40 and brought down its waiting list from 400 people in July last year, to just over 100, allowing it to now provide better, evidence-based, support.
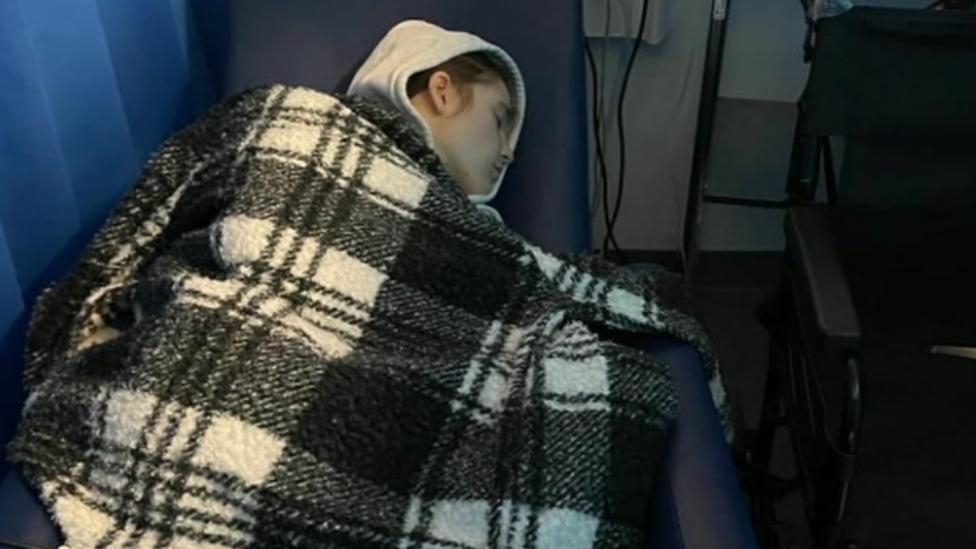
Tia was admitted to hospital on multiple occasions
But now on her way to recovery, Tia said she is worried for anyone else that has recently been diagnosed.
"EDHC has been vital to my recovery. They are the people I trust the most and they believe in me," she said.
"When things do get hard, I'm not going to have them there. It's just a bit daunting and I don't think it has really sunk in yet.
"I'm also upset that some people aren't going to get the same opportunity as me to recover in their safe place, at home.
"The fact that so many other young people and adults that can't do it themselves are going to have to in the future [is upsetting]."

Sally Monkhouse is trying to raise awareness of the "wonderful" work EDHC have done and wants AWP to look at it again before scrapping it
Sally Monkhouse, 74, said she is "devastated" the service is ending.
Her partner has had anorexia for more than 60 years and has also been receiving support through the EDHC.
She said the loss of the service is going to have a big impact on both her partner and herself.
"My partner has given me permission to say they wouldn't be alive today if it wasn't for this wonderful, wonderful service," said Ms Monkhouse, who lives in Chew Valley.
"What is so special about it is people can go on living their lives whilst they're being healed, they're living in their homes, they are being treated in their homes, they can continue education, parents can continue parenting their children safely, people can earn a living while they are doing it.
"I think it is a transferable model, it could go into all sorts of areas of mental health and I think this is a real missed opportunity and I really hope that they look at it again."
'Richer programme'
AWP said EDHC was brought in whilst wider improvements to the eating disorders services were being developed, including a new early intervention programme.
It is now seeing all urgent patients within two weeks, with everyone referred assessed within four weeks.
This has allowed it to provide more tailored support for individuals, significantly reducing the need for EDHC, it said.
A spokesperson added: "We really don't want people to be on intensive meal support for any length of time.
"It was only meant to be brief intervention and what will now be in place is actually a much richer programme that is addressing the underlying factors which is what meal support in itself can not do."
Support offered will include psychological therapy, occupational therapy, dietetic appointments and a level of meal support which will help people work towards independence and recovery.
If you, or someone you know, have been affected by anything in this article, you can find support at BBC Action Line.

Follow BBC West on Facebook, external, Twitter, external and Instagram, external. Send your story ideas to: bristol@bbc.co.uk , external
Related topics
- Published4 February 2023

- Published17 October 2022

- Published19 May 2022

- Published22 July 2021
