Lupus: 'No-one seemed willing to treat me during Covid'
- Published
Some people living with the incurable autoimmune disease lupus have had treatments delayed or cancelled during the coronavirus pandemic. But they also told Cambridge University researchers they now feel more understood by society, as everyone has had to protect themselves and adapt to a slower pace of life. The BBC has spoken to three patients about their experiences.

'There is always the fear of organ damage'

Anisah Patas was told her symptoms were all in her head for years before she was diagnosed aged 12
In April last year, Anisah Patas was told about a possible shortage of hydroxychloroquine, because it was being considered as a treatment for coronavirus, external.
The 24-year-old from Derby, who relies on the drug to deal with lupus, said the warning was "scary".
When she had a flare-up in December, her GP referred her for an emergency hospital appointment, but it took 10 weeks to come through.
Miss Patas, who is treated at a specialist NHS clinic in London, said: "There is always the fear of organ damage, caused by delays in treatment.
"My GP managed my case with steroids, but I was in a lot of pain, I was exhausted, sleeping hours of the day away."
The steroids suppressed her immune system, making her much more vulnerable to Covid-19.
Eventually she was able to have a telephone consultation and was sent hydroxychloroquine by post, so she could come off the steroids.
Despite the delays and stresses, she has found a silver lining to the pandemic.
"During the lockdowns, we all have to spend a lot of time indoors and everyone is doing the same as me," she said.
"There is a lot more awareness of vulnerable people who need to shield."

'No-one seemed willing to treat me'

Shanise Fowler waited six months to see an NHS rheumatologist in June 2020, who referred her to a specialist team she has yet to see
Shanise Fowler, who lives in rural Cambridgeshire, was so frustrated at delays in her care that she paid for a private consultation.
"No-one seemed willing to treat me and I was being bounced between NHS hospitals and my GP," she said.
She was told she might have lupus in 2010, which remained stable for years, but she said she experienced a lupus flare-up when the pandemic began.
"After I saw the private consultant, I was given hydroxychloroquine and steroid immunosuppressants to help me get back on track," she said.

Shanise often gets a rash that is a symptom of the disease, but many lupus symptoms are invisible
The 25-year-old, who works for a housing association, said the lockdowns had provided "an opportunity for reduced social activity" and "more flexible working arrangements from home - otherwise I would have collapsed".
She said she can now tell her manager when she needs to step back from work and is able to catch up later in the day.
"Before I'd have to take half a day off work," she said.

What is lupus?
It is an incurable immune system illness
It can produce many symptoms and can lead to irreversible organ damage
Many people with lupus are unusually sensitive to the sun, which can trigger a skin rash
Affected organs include kidneys, skin, brains, hearts and lungs. Almost all patients experience pain and extreme fatigue
Nine out of ten patients are women and it is more common in people of black, Asian and minority ethnic heritage

'Shielding is normal for me'

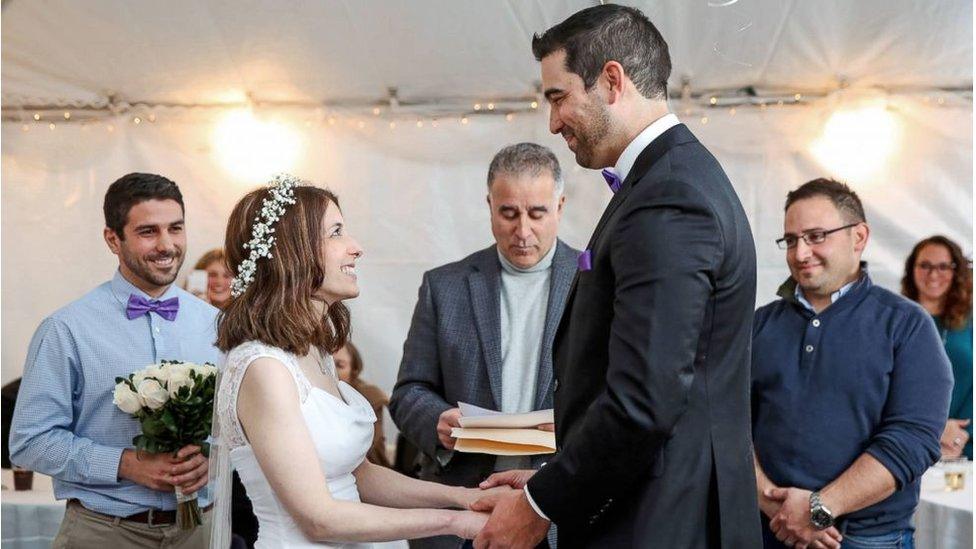
John Webb battled with ill-health for seven years before a blood test revealed he had lupus
John Webb has just been told his appointment with his rheumatologist, which he normally has twice a year, has been cancelled.
The letter arrived shortly after he learned the immunosuppressant drug he has been taking has caused liver damage, so he now needs to move to a new medication.
It took seven years of ill-health, regular GP visits and time off work before he was diagnosed with lupus in 2010.
The 62-year-old, who lives in St Neots in Cambridgeshire, took early retirement on health grounds from his job with BT.
"My tongue-in cheek response to people is that shielding is normal for me," he said.
"We don't go abroad, we can't plan anything as I don't know how I'll feel each morning and I have to be careful in the sunlight as it can trigger a reaction."

'Lupus patients feel abandoned'

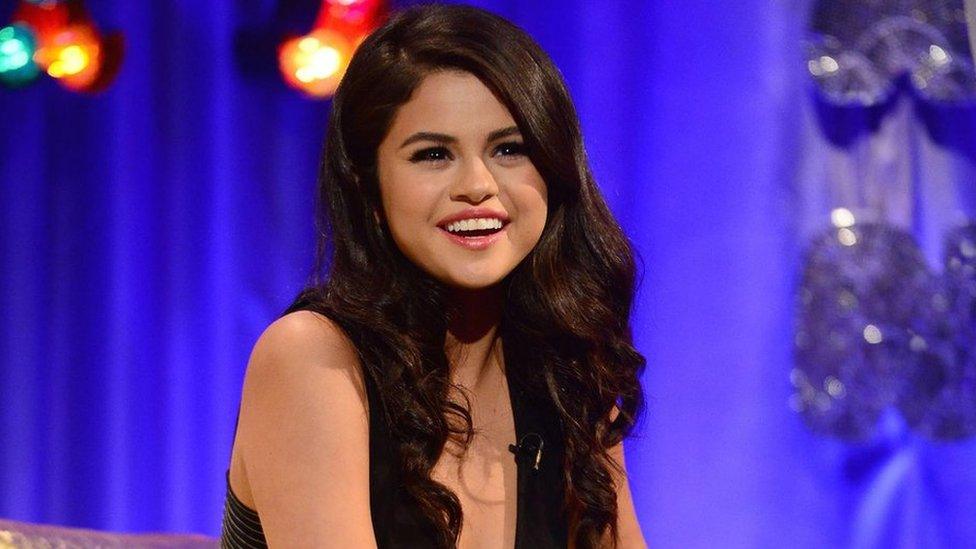
Researcher Melanie Sloan also has lupus and has been in hospital several times during the pandemic
Many of the specialists who usually look after lupus patients have been redeployed to help Covid patients, according to Melanie Sloan, a Cambridge University research associate.
She is leading a research team, external which includes rheumatologists, behavioural scientists, expert patients and the charity Lupus UK. She also has lupus herself.
Data gathered during the pandemic has revealed "lupus patients feel abandoned and more medically insecure, external, especially when they kept trying to get hold of their doctors in an emergency and some didn't even answer these calls for help", she said.
But some health and wellbeing measures, external actually got better during the pandemic.
She said the feeling that the rest of society was "in the same boat due to lockdown reduced [the] pressure and guilt" and she had "more chance to rest without feeling judged for not being able to live a 'normal' life".
She hoped that lupus could benefit from the type of support that was emerging for "long Covid" patients and believed they shared similar life-changing symptoms like severe fatigue and pain.
Paul Howard, chief exec of Lupus UK, said more people had contacted the charity for help during the pandemic, because they had not been able to access their normal support systems.
He said: "We've been hearing from a lot of people with lupus struggling because they are unable to speak to their rheumatologist and even get essential tests.
"More positively, it also shows that being able to adapt to a slower pace of life and less societal pressure to attend the workplace and work from home has a good outcome for day-to-day health."
The BBC has asked NHS England for a response.

Find BBC News: East of England on Facebook, external, Instagram, external and Twitter, external. If you have a story suggestion email eastofenglandnews@bbc.co.uk, external
- Published6 February 2019

- Published29 March 2018

- Published8 January 2018
- Published14 September 2017

- Published8 October 2015