Mental health support gap is no man's land, says Cambridgeshire GP
- Published

Sarah from Cambridgeshire said her son felt "abandoned" by NHS mental health services
A mother has said her son fell into an "abyss" when his care was halted for several months while moving from child to adult mental health services.
Sarah, not her real name, said he was later taken to hospital after suffering a severe mental health crisis.
GP Dr Tamara Keith said some young patients were stuck in "no man's land" between the two services.
Cambridgeshire and Peterborough NHS Foundation Trust (CPFT) said it was "dedicated to providing treatment".
Sarah, who wants to remain anonymous to protect her son's mental health, said he was being treated by a psychiatrist under the trust's child and adolescent mental health services (CAMHS) before being discharged aged 17 and referred to adult services.
His medication continued but his therapy stopped, she said, and after months of waiting with no other treatment, his condition declined to the point where he was admitted to A&E.
"In that period of time, he felt abandoned," Sarah said.
"He felt that he wanted to get some help but couldn't; he hadn't been accepted by adult services but had been discharged by children's services.
"Everyone knew that my son existed but he was handed from one to an abyss before being picked up by the other."

If you have been affected by the issues raised in this article, help and support is available via BBC Action Line.

Several months after the acute episode, he started one-to-one therapy through adult mental health services.
The delay was "incredibly harrowing", Sarah said, and the experience left her needing to access therapy.
"If you're watching somebody you love [...] suffer, it doesn't matter what that suffering is [...] you feel powerless to do anything about it, you absorb it yourself," Sarah said.
Children needing mental health treatment come under CAMHS, and the move to adult mental health services often starts at 18 years old, with some NHS trusts starting it earlier at 16.
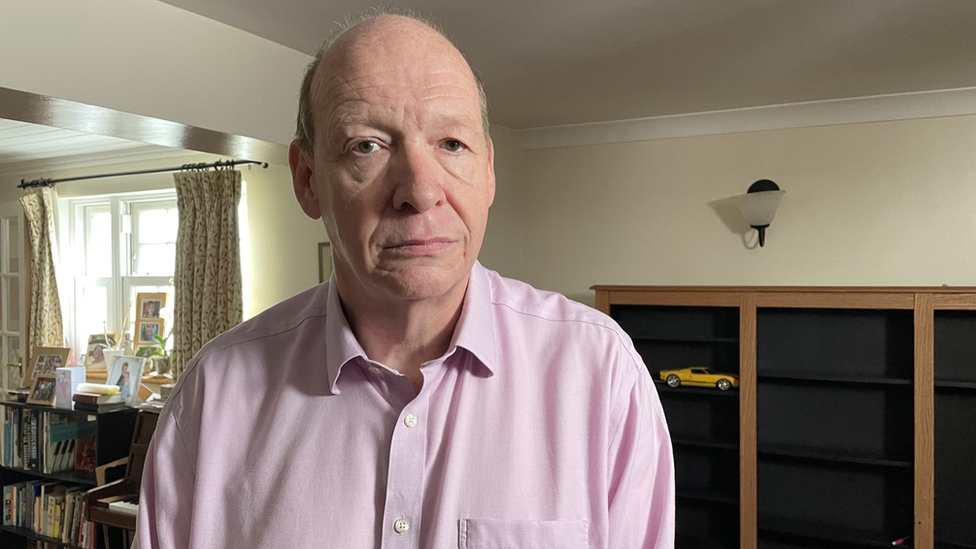
Dr Tamara Keith, from Bottisham Medical Practice, in Cambridgeshire, said the gap between the two services had been a problem since she became a GP eight years ago.

Dr Tamara Keith said young people stuck in the treatment gap felt let down but it was "out of my control"
"You hit 17 and the child services will no longer see you, and you then get put at the bottom of the queue for the adult services, so it's a bit of a no man's land.
"We're seeing frustrated patients, frustrated parents, and it's upsetting for us," she said. "We feel a bit stuck as well."
She said CAMHS staff tried their best but their "hands are tied".
Danny France, 17, from Stetchworth in Cambridgeshire, was being transferred from CAMHS in Suffolk to adult services in Cambridgeshire when he died in April 2020.

Danny France took his own life in April 2020
Assistant coroner for Cambridgeshire Philip Barlow said in a prevention of future deaths report, external that Danny was "repeatedly assessed as not meeting the criteria for urgent intervention".
His father, Alastair France, said it was "incredibly disappointing" to hear the gap was still an issue, and described young people in it as "the forgotten children".
"If they're going through the same hoops that Danny tried to jump through and getting nowhere, then there's something wrong," he said.
Tom Madders, from the mental health charity YoungMinds, said systems to support young people during the transition to adult services were "inconsistent".
"For those approaching their 18th birthday, it can be particularly uncertain," he said.
"Young people have told us moving from child to adult mental health services can feel like a cliff-edge as they try and navigate this transition.
"Young people must be able to access support when they need it," he said.
Alastair France said he wanted better communication between services to "allow some continuity of that care" for young people
Sarah said her son was in a better place now and continued to receive NHS support - but she wanted to see a "seamless transition" put in place for others.
CPFT said its teams worked closely with young people and their families including peer support workers who could share their experiences.
A CPFT spokesman said: "We are committed to improving the transition of young people to adult mental health services, and extending services to support those aged up to 25 is a key part of the NHS Long Term Plan."
An NHS England spokesperson said there was "still work to do to ensure everyone receives the best possible care".
"Systems are making good progress - with nearly all having partially or fully implemented measures to remove age-based thresholds for accessing care or improve joint-working to better support young people as they transition to adult services," they added.
A spokeswoman for the Department for Health and Social Care said: "The Mental Health Implementation Plan [aims] for all local areas to have a comprehensive 0-25 model in place by March 2024."

Follow East of England news on Facebook, external, Instagram, external and Twitter, external. Got a story? Email eastofenglandnews@bbc.co.uk, external or WhatsApp us on 0800 169 1830
Related topics
- Published28 February 2022

- Published25 February 2022
