Cancer surgery survivor helping researchers in new study
- Published
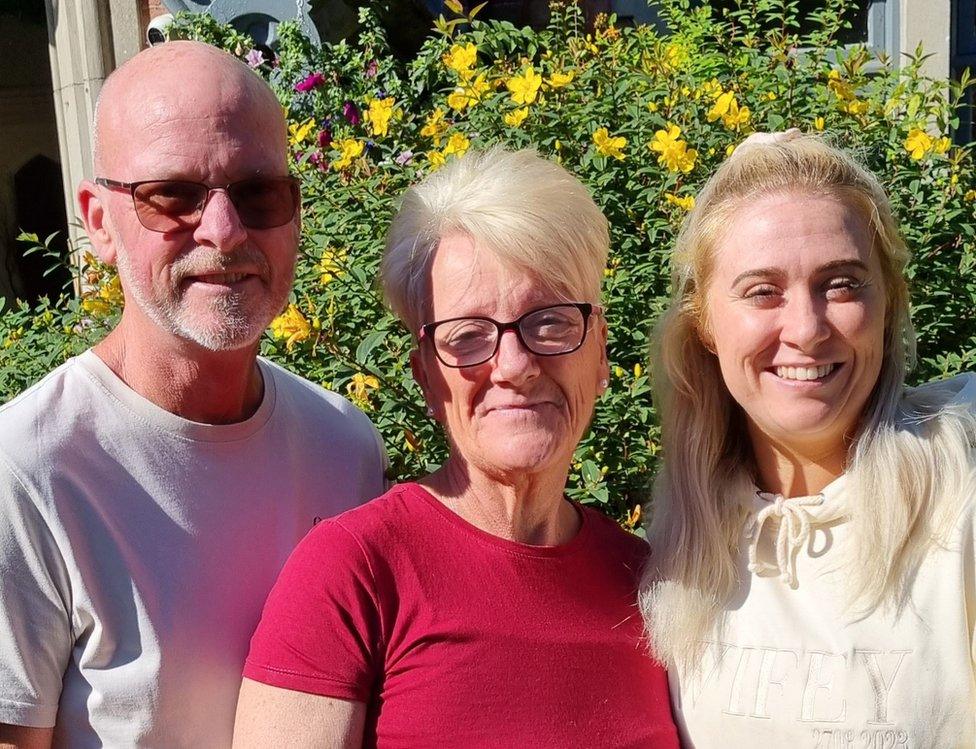
Sharon Applin (pictured with husband Sean and daughter Kelly) has been left with a life-changing condition
A cancer patient who had to have all the organs within her pelvis removed is at the centre of a research project designed to improve future treatments.
Sharon Applin, 58, from Wimborne, Dorset, is taking part in the study at Southampton General Hospital.
She said she wanted to ensure the "best reconstruction and quality of life" for other patients.
About 4,000 UK patients are treated for advanced pelvic cancers every year, but the procedure poses challenges.
The Reconstruction in Extended MArgin Cancer Surgery (REMACS) study, funded by Planets Cancer Charity, takes a closer look at patients' quality of life afterwards, and aims to find the best methods of reconstruction.
Ms Applin, who was previously treated successfully for a skin cancer in 2020, started experiencing bleeding, diarrhoea and severe pain last year.
It turned out to be from cancer affecting her abdomen and pelvis, for which she required major surgery known as a total pelvic exenteration.
It involved removing her bladder, rectum and part of the colon, her uterus, fallopian tubes and ovaries, and part of her pelvic and pubic bones.
Skin and muscle was also removed from her abdomen to fill in those areas removed.
'Forever grateful'
"[It was] explained very clearly that without major surgery I had only six months to a year to live," Ms Applin said.
"To come round from the operation and have the realisation of what had been removed and what I didn't have anymore was an emotion I never wanted to experience."
However, she said she was "forever grateful" to have had the successful operation, though it left her with a "life-changing condition", and the need for two stoma bags.
Ms Applin said she now had to rethink her daily routines.
She said: "Where am I going and is there a toilet nearby? Can I park my car nearby? How long am I going to be away from home?
"I need to make sure I have my stoma bags stocked up just in case of an emergency and a change of clothes in case of any leaks... this is a mental strain all the time and has changed my life."
While in hospital she was told about the study and volunteered to help.
"Being involved has helped me come to terms with what I have had done, what I have been through, and to understand how pelvic exenteration is done," she said.
"Providing my own input into what I feel is important to the operation - and seeing what others think - will hopefully help people undergoing treatment and surgery in the future."
Charles West, colorectal surgery research fellow at the University of Southampton, said the operations were "very invasive and leave large wounds that can cause complications and reduced quality of life for patients".
He said Sharon's participation had been "invaluable" and would "undoubtedly lead to improvements in quality of life for patients in the future".

Follow BBC South on Facebook, external, Twitter, external, or Instagram, external. Send your story ideas to south.newsonline@bbc.co.uk, external.