Leeds and Bradford Hospital errors in care of mother whose baby was stillborn
- Published

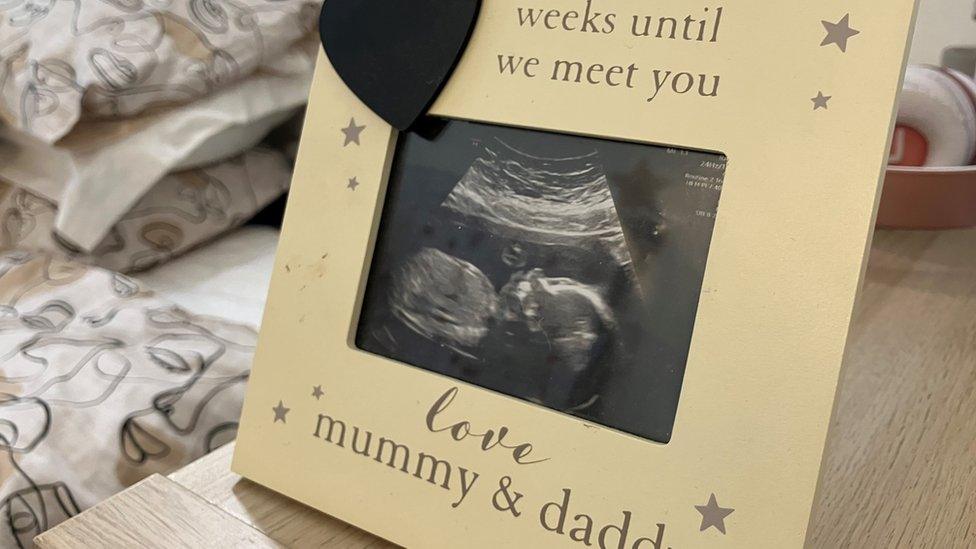
Lauren Caulfield was in labour when she was told her baby daughter had died
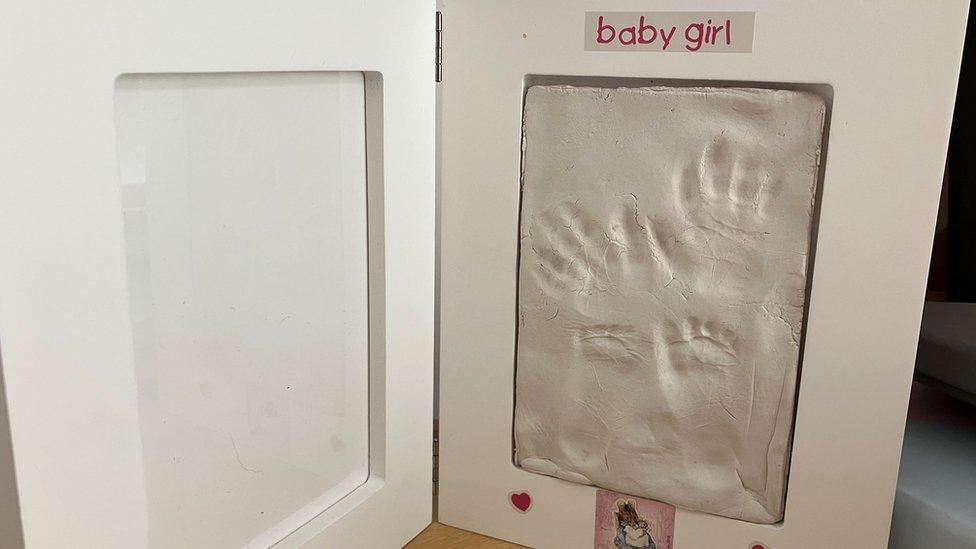
A mother whose baby daughter was stillborn said she was heartbroken when hospital staff disposed of the placenta before it could be tested.
Lauren Caulfield's daughter Grace died in the days before she was born at Leeds General Infirmary. Tests on the placenta may have provided answers.
An investigation found other errors in her care at the hospital and at Bradford Teaching Hospitals Trust.
Both hospital trusts said they have made changes since Grace's death.
Ms Caulfield was in labour in March 2022 when she was told her baby had died.
A post-mortem examination found Grace had died from a sudden lack of oxygen two or three days before birth but the reason for this could not be identified.
Analysis of the placenta could have provided a possible explanation and helped with future pregnancies, but it was disposed of in error.
An investigation by the Healthcare Safety Investigation Branch found failings in Ms Caulfield's care
"It breaks me," Ms Caulfield said.
"Every single day it breaks my heart knowing that this life has gone and we will never know why."
Ms Caulfield's care was provided by Leeds Teaching Hospitals Trust and Bradford Teaching Hospitals Trust during her pregnancy.
An independent report by the Healthcare Safety Investigation Branch (HSIB) found several other failings in her care.
These included the baby's growth not being consistently monitored because of the use of different systems.
Investigators said there were two occasions when growth scans should have been requested but referrals were not made.
The report found that had Grace's growth rate been correctly diagnosed, it "may have altered the outcome for the baby".
'Unimaginable pain'
"It could have been escalated and I really do believe we really could have changed the outcome," Ms Caulfield said.
"There was no reason for her to die. She didn't need to die.
Ms Caulfield was also left without postnatal care for 15 days following the birth, due to an error in the discharge process.
"I permanently feel like there's a part of me missing. It's an unimaginable pain that I don't think anyone could understand unless they have experienced it themselves."
Ms Caulfield has begun studying to become a midwife in the hope of helping others to avoid a similar experience.

An independent report said there could have been a different outcome if baby Grace's growth rate was diagnosed
Dr Magnus Harrison, chief medical officer at Leeds Teaching Hospitals NHS Trust, said: "There was an error which led to the disposal of Lauren's placenta and could have assisted in understanding why Grace died, and for this we are very sorry."
He said the trust had "implemented the recommendations outlined in the HSIB report".
Changes included a new procedure for analysis of placentas and upgrades to the digital maternity system to improve communication between hospital trusts sharing patient care.
"Our care fell short on this occasion and we remain committed to providing safe, integrated care across our maternity service," he said.
Leeds Teaching Hospitals Trust has apologised for errors in Ms Caulfield's care
A spokesperson for Bradford Teaching Hospitals Trust said they had "completed the actions identified" following the investigation into Grace's death."We have also worked closely with Leeds Teaching Hospitals on joint learning points around sharing information between different NHS organisations involved in delivering maternity care," they said.

Follow BBC Yorkshire on Facebook, external, X (formerly Twitter), external and Instagram, external. Send your story ideas to yorkslincs.news@bbc.co.uk, external.