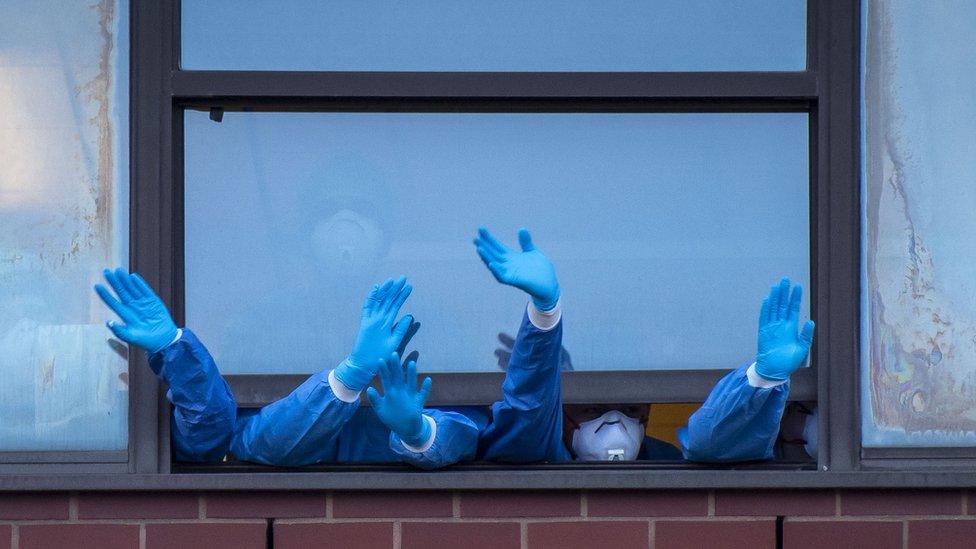
Covid-19: 'One medic saw eight people die in a single shift'
- Published

Claire Goodwin-Fee: "People are being pushed to the brink"
Coronavirus has changed many people's working lives for the worse. Many of us have been isolated from our colleagues; others have been made redundant by employers citing the costs of the pandemic.
In the NHS and in care homes, though, the pressures have perhaps been the most intolerable. Ten months of Covid-19 has left many healthcare professionals' mental health at breaking point, according to Claire Goodwin-Fee.
The Frontline19 organisation she runs with fellow therapist Ellen Waldren has received more inquiries in the past week than it did in the whole of December. The free service, external, which is funded by donations, is currently helping about 1,800 healthcare workers a week.
Here, in her own words, Claire explains the scale of the mental health problem she is witnessing.
'People are feeling sick about going into work'

I'm waiting for the headline that says: 'Doctor takes own life because of the pandemic'. It is going to happen. If not today, it'll be soon because they are on their knees - and they want people to know that.
There is a huge amount of anxiety. People are feeling sick about going into work and what they're going to see.
They're seeing multiple deaths on a shift - someone the other day saw eight or nine people pass away. Someone else got in contact with us and said 'I know by the time I go back on my shift tomorrow six of my patients won't be there. How do I manage that?'
Frontline staff are not given any time to process it, so it's repeated, trauma after trauma after trauma. And yet these people go home, have their dinner, try and relax as best they can, get up, get washed - all the time worrying about if they're going to infect the people they live with.
Some people will function on autopilot, until such times when they physically can't, but they are being pushed to the brink.
'He put his head on the desk and sobbed'

London-based Frontline19 was set up by Claire Goodwin-Fee and Ellen Waldren to offer free therapy to healthcare professionals
We had a doctor who has a young family but is keeping separate from them, who was traumatised by the fact that he had lost two of his colleagues to Covid. On one shift he lost five patients pretty quickly into the shift and as soon as those beds were free, they filled up with more coming in.
He then had to phone up the relatives of the people who had sadly passed away. He said he wasn't equipped to do that - he didn't know what to say. He put the phone down and put his head on the desk and sobbed and he said: 'I can't manage it any more.'
Paramedics are getting called out on shifts where they're going to houses and they're telling us that they look at the people and they know they're going to die because they're so sick.
One of those events can happen and you could probably manage it with the right support. But this is happening numerous times a shift. How is anyone supposed to cope with that?
'It's horrendous out there'

Care home staff have really struggled throughout the pandemic.
The dedication and compassion to the people they look after is amazing; it's inspiring. A lot of them moved into the homes because they didn't want to risk the contamination of bringing things into the home.
Some have said they've lost 70% of the people in these homes. They've washed and dressed their bodies and these are people they've had relationships with; they've fed, they've looked after, they've talked to, they've shared memories with.
Then they have to dress them for their final moments, pick up their coat and go home or go upstairs and try to relax - how can anybody cope with that?
It's horrendous out there. It's absolutely horrendous and the care homes were ignored for a long, long time and they desperately need support.
I remember - it broke my heart - we had an email through at the start of the pandemic where someone very tentatively said: 'I don't suppose this service applies to those in care homes?' And I said 'yes of course it does, why wouldn't it?' And they said 'because we're not a professional service'.
It's heartbreaking that these are people who are professionally trained, who are saving the lives of numerous people, are being treated so poorly.
'NHS staff don't want to be clapped'

You've got doctors living in garages or hotels and are keeping separate from their loved ones because they know that this new strain is much more contagious so they need to protect them, while being mums and dads, grandparents and all these different things.
Their colleagues are dying around them and then you have these people saying 'Covid isn't real' or 'you've got time to do TikTok'.
I would love for people to see actually what's really going on in these wards. It's horrific.
We had a conversation with a few people this week about Clap for Carers, and I know it's meant in the best possible way but people are furious about it [returning]. They don't want to be clapped. What they want is for people to stay home and, if they have to go out, wear a mask.
'The system is starting to break'

We've had people that have been part of terrorist situations and they've never had support. They've now gone into this pandemic and they've got something called complex PTSD, which is when someone has seen numerous traumatic situations. We're getting a lot more people with that.
We're getting people who have post-traumatic stress disorder and yet a lot of them are still working.
There are people off sick with complete breakdowns. We've spoken to people who have been sectioned because they are so traumatised by what they're seeing.
The system is starting to break already but it's going to get worse.
In October, sick days in the NHS due to mental health was 500,000 days. This is going to be a bigger problem in the long term. This needs to halt now.
'What's going to happen to these people?'
It's amazing that people are reaching out for help, and of course we want to keep doing that, but at times it feels overwhelming. The need is so great. I think it's been that way for a while but obviously the more we talk about what's happening and share how difficult things are - and some people are really having horrific situations that they're having to work through - that increases the amount of people who seek support.
The positive side is with the right funding we could scale this. The psychotherapists [to whom Frontline19 refers healthcare workers] are all qualified and insured so they know what they're doing.
My concern is if we don't become sustainable and receive funding, in the long term what's going to happen to these people, the very backbone of the UK?
I'm really hoping that we can secure funding from the government so we can continue to support the amazing people in the NHS.
I strongly believe that we owe it to each other to look after one another. This could be a great time of connection and support but the changes need to be now.
As told to Sonja Jessup; produced by Rebecca Cafe


Claire Goodwin-Fee's advice to frontline staff:
Talk to people; reach out to us - we're a very easy service. Don't wait until you're on your knees. There's a culture within the NHS about not talking about how you're feeling. That has to change now and that has to be a long-term change.
Don't blame yourself. It's a very natural response for anyone who has been through a traumatic experience to experience trauma. There isn't anything you're doing wrong and it's a very natural response to an abnormal situation.
There are resources out there - yes, they are busy but don't let that put you off.

A Department of Health and Social Care spokesperson said: "Supporting the mental health and wellbeing of health and social care staff is a top priority, and we understand the huge pressures they face, particularly during this unprecedented pandemic."
The spokesperson added that the department had invested £15m to support the wellbeing and mental health of staff and developed a national support service for those most vulnerable to severe trauma. A mental health hotline, external, practical support and specialist bereavement and psychological support services were already available to staff, and since October the National Institute for Health Research has funded a range of research projects dedicated to understanding the impact of the pandemic on the mental health of frontline NHS staff, the spokesperson said.
"We would urge anyone struggling to come forward and speak to a colleague, their occupational health team or to call the helpline so that they can get the help they need."

TESTING: How do I get a virus test?
SUPPORT BUBBLES: What are they and who can be in yours?
TEST AND TRACE: How does it work?
- Published21 October 2020

- Published12 August 2020
