East of England Ambulance Service: Inside a 999 control room
- Published
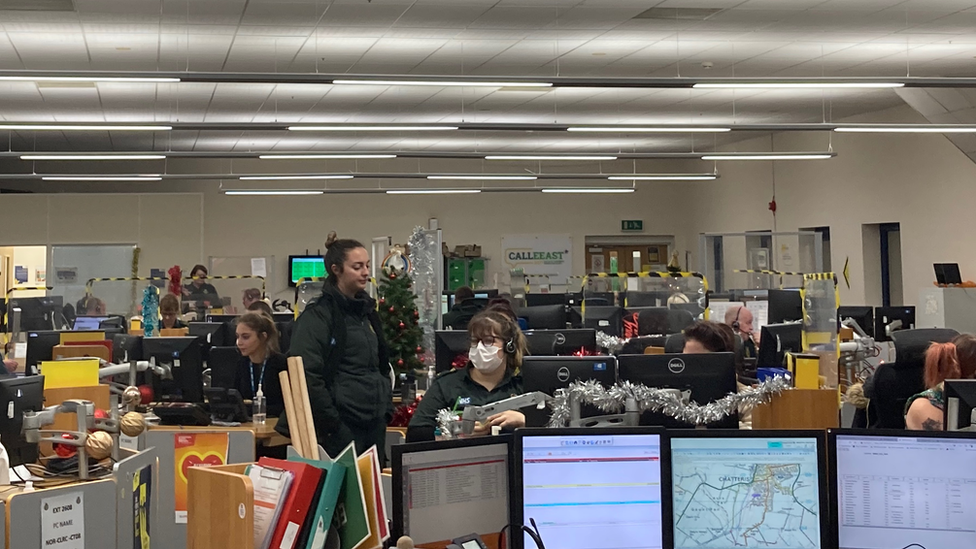
The East of England Ambulance Service control room in Hellesdon, near Norwich, is one of three in the region
Faced with answering thousands of calls a day, often concerning life-or-death emergencies, what is it like to work in an ambulance control room?

'Look, we are struggling'

Duty manager Thomas Pont is part of a team handling 999 calls in the East of England
"We've now got over 100 calls outstanding, waiting to be responded to," says Thomas Pont.
It is Wednesday and the 30-year-old is on shift as duty manager at the East of England Ambulance Service's control room in Hellesdon, near Norwich.
The trust has three control rooms, with others in Chelmsford and Bedford.
The Hellesdon base dispatches to Norfolk, Cambridgeshire and Waveney, in Suffolk.
The last few days, he says, have been particularly difficult, with delays getting patients into hospital.
"We're not able to respond to patients so we then start stacking up, stacking up and stacking up," he says.
Calls are categorised from one - for the most serious and anything immediately life-threatening - to four, which are non life-threatening emergencies requiring transport to hospital.
Mr Pont says they should respond to category two calls within 40 minutes but they are taking 90 minutes - and they are telling those in the less serious categories an ambulance may take 15 hours.
If a doctor calls for a patient who needs to go to hospital, but it is not urgent or time critical, they will be advised it will take 22 hours, he says.
He adds they also advise people that, if they can, they are better getting themselves to hospital.
"That's the reality of the situation we're in at the moment," says Mr Pont.
"This is making the best of a bad situation.... It's about us being really open and transparent with people and saying, 'Look, we are struggling'."

'My head can feel like it's spinning'

Dispatcher Chantelle Cornwall's job is to get the most appropriate resource to patients by juggling the priority levels of calls
"It gets frustrating looking at jobs and you can't do anything," says dispatcher Chantelle Cornwall.
The 43-year-old's job is to get the most appropriate resource to patients by juggling the priority levels of calls. She is in charge of dispatching 49 crews.
"You need to be able to multitask. Sometimes, on a crazy day, my head can feel like it's spinning. I have to be able to monitor everything," she says.
Ms Cornwall says delays at hospitals can be "so frustrating" if it means crews are stuck there.
"It can be difficult, no-one likes to have calls uncovered. It's stressful when you can't cover your own call or everyone is busy dealing with incidents or is stuck at hospital," she adds.
"If you haven't dispatched on all your patients by the time you leave, you feel like your job isn't complete."

'I sprint until I try to go home'

Advanced paramedic Richard Davis says everyone in the call centre is gives "everything" for the patients who call
To try to reduce the number of calls waiting, the ambulance service is introducing a scheme to use more advanced paramedics or advanced practitioners to get "the right help to the right people".
Richard Davis is one of the advanced paramedics on hand.
"It's all about trying to get the right care to the right patient as swiftly as possible," he says.
Mr Davis, who has worked in the ambulance service for 20 years, describes the workload as "stressful".
"I walk in that door and I sprint until I try to go home," he says.
He is full of praise for his colleagues.
"It's fundamentally an amazing team and I'm not sure they get the appreciation they rightly deserve for what they do, put up with, go through and come back tomorrow and do it all again, day in, day out," he says.

'The increase in head count has helped'

Rob Hazell, who is in charge of recruitment, says they have increased the number of call handlers by 136% within 12 months
The ambulance service is improving its call response times after a recruitment drive, says Rob Hazell.
The 30-year-old, who is in charge of recruitment, says the number of call handlers has increased by 136% within 12 months, something which, he says, has improved the average call pick-up time.
He says in July, the average call pick-up time was one minute and 18 seconds. In November, it was 21 seconds.
Calls waiting for more than two minutes per day were 804 in July. In November, it was 121, he adds.
"The increase in head count has helped massively," he says.
"I certainly feel that recruitment and retention has arguably had the biggest impact on what we have been able to serve our patients in terms of calls pick-up and calls waiting."
But, he says, the trust still has a challenge with retaining staff.
At the start of the year, he says they lost on average four call handlers every week. That average is now just below two, he says.
Helping staff feel part of a team and a well-being culture has improved retention, says Mr Hazell.

'The green family'

Senior call handler Melissa Rowlands joined the ambulance service at the start of the pandemic
Melissa Rowlands, 39, joined the ambulance service in March 2020 as a call handler, two months after being made redundant from her previous role.
Now a senior call handler, she says the death of someone she knew "changed her perspective" and made her "realise how you really want to take care of people".
"It all made sense," she says.
She says there are calls that "stay with you".
"I can talk to my partner if I need to but, at work, the green family as we call it, we understand what each other are going through," she says.
"I love my job. It can take a toll but we are trying the best we can."
With Christmas parties, the World Cup and the current cold snap, Ms Rowlands has a message for people heading out.
"Take a coat out with you, be sensible, have a plan about how to get home," she says. "We are not there to be a taxi service."

Find BBC News: East of England on Facebook, external, Instagram, external and Twitter, external. If you have a story suggestion email eastofenglandnews@bbc.co.uk, external
- Published31 October 2022

- Published20 October 2022

- Published3 October 2022
