Homecare: Covid self-isolation and low pay creating staff shortages
- Published

Nick Flynn, who has cerebral palsy, said he would not be able to live at home without the help of Carewise Northampton
A recent survey showed two-thirds of homecare providers are turning away new care requests due to staff shortages. The BBC caught up with carers in Northamptonshire to find out why.
Just a week into the new year, critical service providers in Northamptonshire declared a major Covid incident.
The onset of Omicron had led to more social care, hospital and emergency service workers having to self-isolate.
When the major incident was declared it was estimated around 10% of front-line service staff were absent from work.
The situation has eased slightly since, but that did not stop West Northamptonshire Council's chief executive Anna Earnshaw revealing the authority is expecting a further six months of pressures on social care as a result of Covid-19.
The county's problems are symptomatic of nationals issues, including for providers of homecare.
Figures from the Homecare Association, external said local authorities in England currently have 400,000 people on waiting lists for assessment.
And a survey from The National Care Forum showed two-third of homecare providers are turning away new care requests due to staff shortages.

'The council phone us on a daily basis'

Helen Kennedy says Carewise Northampton is getting increasing referrals from social services
Helen Kennedy is a care worker at Carewise Northampton which is a private, family-run company which has been operating for nearly 15 years.
Clients include elderly people (one is a spritely 102-year-old), those with severe disabilities and learning difficulties, and people with brain injuries.
Among them is Nick Flynn, who has cerebral palsy.
He says the Carewise team help him get up each morning and go to bed at night.
"Without their help I couldn't be here," he says about living at home.
Ms Kennedy says workers are "very busy" due to staff shortages as a result of people having to isolate after contracting Covid or being in contact with someone with the virus.
She says the company has also had increasing referrals from Northamptonshire's two councils.
"The council phone us up, sometimes on a daily basis, because they have clients they are unable to find care for," she says.
"We're helping them out, but we need more staff."

'We could use three times the staff'

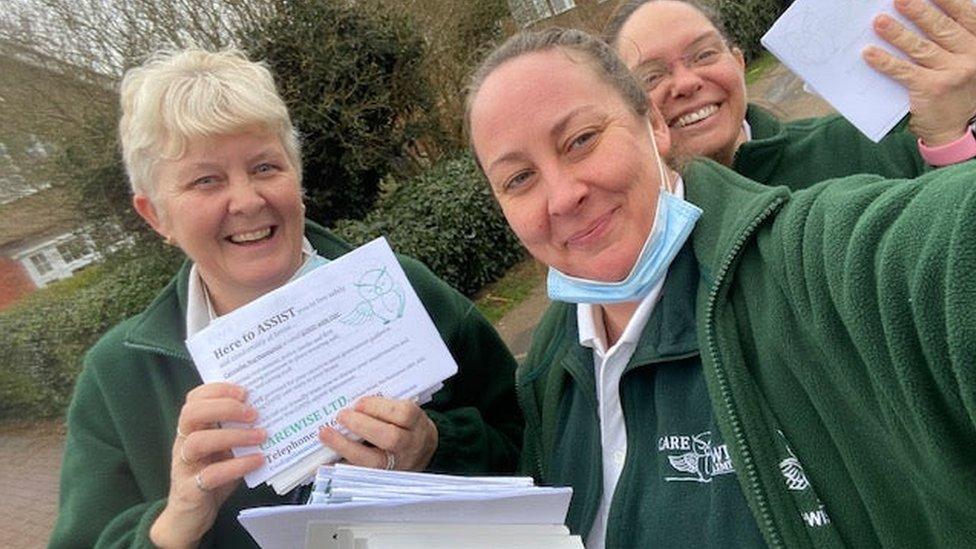
Pam Passmore has been redeployed to visit clients due to staff shortages
One solution employed by Carewise has been to redeploy office staff in the field, including care co-ordinator, Pam Passmore.
"If the care needs covering, that's our priority," she says.
"We're trying to recruit staff, but it's very difficult. We could use three times the staff we have."
Despite the pressure, Ms Passmore says her job is hugely rewarding.
"We do everything a person needs, but it's like visiting your grandma or granddad."

'They can't do more without being exhausted'
All of the staff at Carewise Northampton have been double-vaccinated and have had or will be having booster jabs
Chairman Justin Jewitt said the coronavirus pandemic has made the work Carewise does "four times as difficult".
Carewise staff are taking lateral flow tests every day and PCR tests twice a week. They are also double-masking with every client, and new masks are used for each visit.
Mr Jewitt says all of the care workers have been double-vaccinated and will all have a Covid booster jab, something he calls "essential for our duty of care".
Despite that he says staff self-isolating has increased pressure on the front line.
"Even today one of our care workers had to go and self-isolate because her daughter has isolated," he says.
"Our people are out there seven days a week, 365 days a year for our clients.
"They can't do much more without being absolutely exhausted."
Mr Jewitt says recruiting carers is "a fundamental challenge," with pay a major issue.
A third of Carewise's clients come through social services, with the company paid by the government via local councils.
"Since austerity, the government has cut back to below 30% of what they were funding then," Mr Jewitt says.
"They haven't put in enough money to enable us to pay a reasonable wage."
He says care worker pay largely comes from fees paid by private clients, but that can only go so far.
"We need social services to be well funded, then we can pay care workers positively," he says.
While Mr Jewitt welcomes government plans for a £162.5m care workforce retention and recruitment fund, he says the are currently "abstract" and there has been no "concrete activity".

'Funding squeeze means people are neglected'

Dr Jane Townson said funding pressures have led to people being neglected
Dr Jane Townson, the chief executive of the Homecare Association, also points the finger at austerity.
She says funding given to councils by central government has been "progressively squeezed" leading to people being "neglected at home, left on their own in the community and unable to get out of bed or feed themselves".
"That person ends up being blue-lighted to hospital," she says.
A Department of Health and Social Care spokesperson praised the "dedication and tireless work of health and social care staff throughout the pandemic".
The government says it is investing £5.4bn in social care over the next three years, while "working to ensure we have the right number of staff with the skills to deliver high quality care to meet increasing demands".

Find BBC News: East of England on Facebook, external, Instagram, external and Twitter, external. If you have a story suggestion please email eastofenglandnews@bbc.co.uk, external
Related topics
- Published19 January 2022

- Published18 January 2022

- Published7 January 2022
