Families call for public inquiry over 'unsafe' maternity units
- Published

An inquest found Wynter Andrews, who died 23 minutes after being born, may have survived if "multiple missed opportunities" were spotted by staff
Two families whose babies died at two hospitals have called for a public inquiry after "serious concerns" were raised over their maternity units.
The Care Quality Commission (CQC) rated the units inadequate, criticising staffing and poor leadership.
Wynter Andrews and Harriet Hawkins died at the Queen's Medical Centre and Nottingham City Hospital in 2019 and 2016 with a coroner and a review condemning the care given.
Their families say action is needed.
The CQC carried out an unannounced inspection in October "in response to concerns raised from serious incidents, external investigations... and coronial inquests".
A report released on Wednesday found numerous issues with low staffing and training, with inspectors told "there were not enough staff to provide safe care".
The impact of this was that jobs were missed and standard of care was poor, according to the report.
The watchdog imposed conditions on the registration of maternity and midwifery services at both the Nottingham hospitals.
Nottingham University Hospitals NHS Trust was also given a warning notice over concerns "found around the documentation for risk assessments and IT systems".

Wynter's death was "a clear and obvious case of neglect", a coroner said
The families of both babies welcomed the CQC's findings.
Wynter Andrews was delivered by Caesarean section on 15 September 2019 at the Queen's Medical Centre (QMC) but died shortly after.
A court heard concerns over her and her mother Sarah Andrews - who was admitted to hospital six days after suffering contractions - were not acted on.
An inquest in October ruled Wynter's death was "a clear and obvious case of neglect".
The hearing also revealed a letter from midwives at the unit to bosses at the trust in 2018 outlining concerns over staffing levels as "the cause of a potential disaster".
Commenting on the CQC report, Mrs Andrews said: "It is quite an upsetting read.
"We do feel the trust doesn't really have the ability to change. They have had opportunities to change, and they made lots of promises but nothing has changed.
"We just want our daughter's life to mean something. We don't get to see them grow up and get married, all those things you expect as a parent."

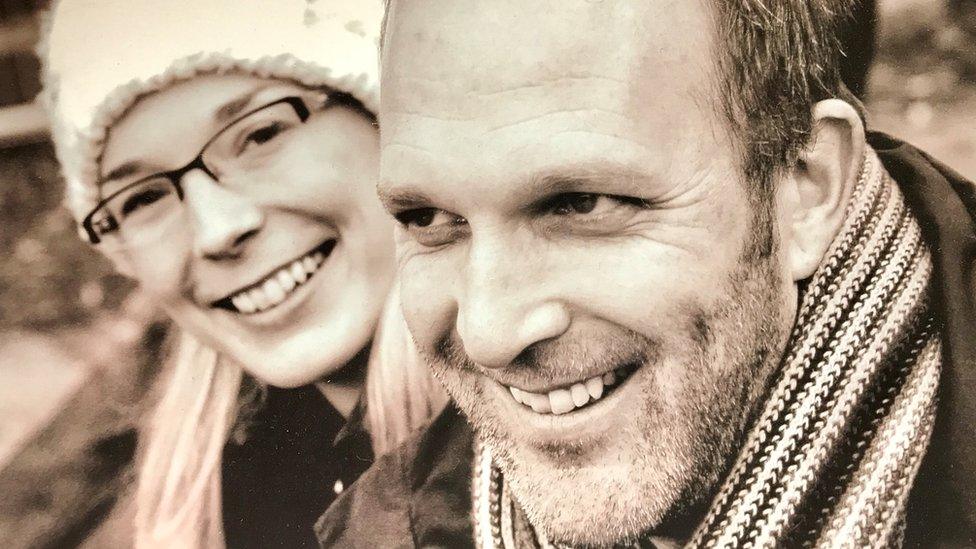
Jack and Sarah Hawkins said Harriet's death in 2016 was "avoidable"
Harriet Hawkins was delivered at Nottingham City Hospital in April 2016, nine hours after dying.
An external review of the case found 13 failures and concluded her death was "almost certainly preventable."
Jack and Sarah Hawkins, who both worked for the trust as a hospital consultant and senior physiotherapist respectively, said: "Since Harriet's death we have continuously tried to raise awareness, through multiple different bodies, that maternity services were unsafe at NUH."
They added: "The CQC report was no surprise.
"We had an independent review which found 13 significant failings and years later the same things are happening."

A review found 13 failures in Harriet's care
Natalie Cosgrove, of Switalskis Solicitors - which is representing the two families - said: "I am exceptionally concerned about the trust's ability to enact change.
"During my investigations there are often promises of protocol changes, but protocols do not change the culture."

Nottingham University Hospitals NHS Trust accepted the CQC's findings
Tracy Taylor, chief executive at the trust, said they accepted the CQC's report, adding improvements have been made including hiring extra midwifery staff and additional training.
She said: "We want to provide the best maternity services for local people, and the priority of our maternity team is to provide safe care to the families they come into contact with every day but we know we haven't always got this right, and we are very sorry.
"We accept the report from the CQC and have already made some immediate changes and will continue to make further improvements, and I would like to reassure local people that we are committed to working to make its maternity service one that we can all be proud of."

Follow BBC East Midlands on Facebook, external, Twitter, external, or Instagram, external. Send your story ideas to eastmidsnews@bbc.co.uk.
Related topics
- Published2 December 2020

- Published7 October 2020

- Published10 January 2018