Why Swindon's Great Western Hospital A&E 'has no space'
- Published

The Great Western Hospital is trying a new approach to A&E delays
As hospitals across the West face long delays in A&E, Swindon's Great Western is trying a new way to ease the strain.
Salisbury District Hospital was the latest this week to warn they are struggling to free up any space for new patients, as NHS bosses across Wiltshire, Somerset, Gloucestershire and Bristol meet to plan for winter.
Medics say the queues in A&E are largely caused by a lack of ward beds, as too many patients are stuck in hospital long after they should have been discharged.
As we await the new health secretary's plans for tackling these backlogs, I joined the team at the Great Western Hospital (GWH) who say they are the first in the country to set up a new control room to get things moving.
"We have no space in the hospital to get our patients up," says Sister Emma Roberts, a senior nurse in the Emergency Department (ED) as she scrolls through a screen telling her there's an estimated twenty five hour wait to do so.
"Winter pressures are coming so I'm sure they're going to get even worse," she says.
Not including the resuscitation area, normally Swindon's ED has 14 beds. On the day I visit, 12 of them are occupied by patients waiting to go up to a hospital ward.

Ambulances are often queuing to unload patients due to a lack of space inside

A corridor is used as an extra ambulance unloading area, but patients are moved to beds not trolleys because of the long waits
That's why there can be long waits with ambulances queuing outside, even though the waiting room can appear quiet.
"Sometimes you really can't do much about it," says Emergency Nurse Philmore James. "It troubles you for sure but we just do the best we possibly can."
The new health secretary Therese Coffey has said tackling ambulance delays is one of her top priorities.
But my time at the Great Western shows the source of the problems is far deeper into the care system.
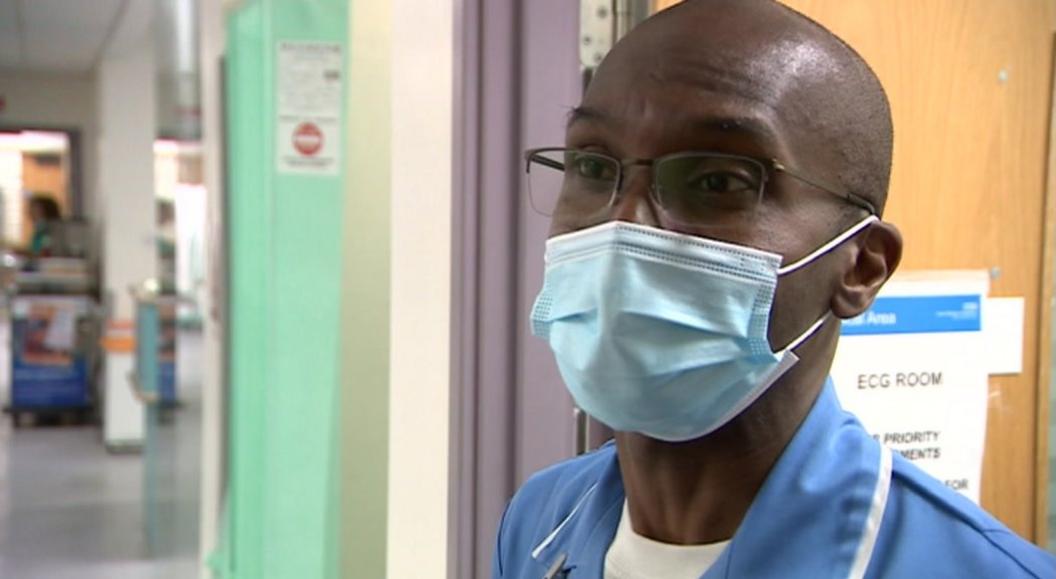
Emergency Nurse Philmore James says sometimes there is nothing he and his colleagues can do see patients more quickly
Emergency Consultant Dr Gareth Clark sets out the issue. "If the wards can't clear patients out they can't take new patients in," he says, "which means when ambulances arrive we haven't got anywhere to put them."
So while ambulances queues grab the attention, the bigger issue is patients being stuck in hospital longer than they should be, as a result of social care being unable to cope.
Dr Clark lets out an exasperated laugh when I ask how to solve that problem.
"There's been a complete loss in the support of community care in the last ten or twelve years or so," for patients who aren't well enough to go home without support, he tells me.
"There needs to be increased funding and support" for his colleagues in social and community care he adds.

Emergency Consultant Gareth Clark says an underfunded social care system is a big reason hospital emergency departments face long delays
As Winter approaches, the NHS's busiest time of year, the Swindon hospital is trying to innovate new ways to get things moving.
Upstairs, from the stack of waiting ambulances, a new control room is taking shape.
"It's revolutionary in Swindon, its going to be like a flightdeck," says the new Coordination Centre's Operations manager Jeanette Etherington. "This will help all our patients receive better, more timely care."

The new control room brings hospital, ambulance and social care teams together to track who is arriving, helping better plan for how they'll leave
Think of it like air traffic control for patients: Big screens with real-time data on who is in what ambulance, who is stuck in a corridor, who should have left hospital by now.
In the room are representatives from each part of the hospital, as well as South Western Ambulance Service and crucially social care teams from Swindon and Wiltshire Councils.
"On my fingertips I know exactly what patients are fit and well to leave," says Head of Clinical Operations Sarah Knight scrolling through one of many huge touchscreens. "How long they've been waiting, what they might be waiting for, and who has ownership and responsibility."
Sarah describes an extreme example recently of her team managing to successfully discharge a patient who'd been stuck in hospital for sixty days longer than needed, waiting for a care home space.
"We know we don't get it right all the time but we're up for listening to ideas and taking on innovation," says Chief Operating Officer Felicity Taylor-Drewe, but "its the same people we're asking to do more and more in the current climate".

The new GWH control room helps Sarah Knight's team keep track of which patients are waiting longer than they should to be discharged
Bosses here know they can only do so much unless the government sorts out the underfunded and overburdened social care system.
The recently-introduced dedicated tax, the Health and Social Care levy, is due to be scrapped.
The Health Secretary for England, Therese Coffey, has confirmed the money needed to free up hospital beds by improving social care packages will have to come from existing funds.
Speaking during a hospital visit in Birmingham after the Conservative Party conference, she said the money for health and social care would "come from general government money, the funding levels aren't changing".
"What we have done, though, is to make sure there is a five hundred million pound discharge fund that will be targeted across the country for this winter."
She stressed that there was huge variation in hospital discharge times - and wanted the worst areas to learn from the best.

Follow BBC West on Facebook, external, Twitter, external and Instagram, external. Send your story ideas to: bristol@bbc.co.uk
- Published16 August 2022

- Published2 August 2022

- Published27 July 2022
