'Doctors discuss my daughter like she's nothing'
- Published

Josselin, centre, is often referred to in medical correspondence in a de-humanising way, like food with "a sell by date", her mother said
A doctor in Cambridge is spearheading a project to help to reform medical language that patients and their families can find upsetting.
Ethicist Zoe Fritz said language that "casts doubt, belittles or blames patients" was long overdue for change.
Sixteen-year-old Josselin Tilley from Wiltshire has charge syndrome that reduces her life expectancy.
Her mother Karen said Josselin's death was often referred to in correspondence "like she's not a person".

Josselin has charge syndrome that reduces her life expectancy
"It's not person-centred at all, it's like she's just nothing," Karen said.
The example she gave was an extract from a typical letter in November that she was copied in to by a community paediatrician addressed to colleagues.
"Death below 35: On discussion with Josselin's mum early death has been discussed with her, and there is plan, discussed with Josselin's mother about a wishes document being done."
"Discussion with family: mode of death: This will be included in the wishes document."
Mrs Tilley, from Westbury, said she objected to the use of language that "very bluntly discusses Josselin's death like she's something going off in the fridge".
Listen to Mrs Tilley chat to BBC Radio Wiltshire about her experience
She said she had endured 16 years of such medical correspondence.

Josselin relies on her buddy dog Stormzy and takes great comfort from him
HCRG Care Group said it was unable to comment on the specific case but said "we would never want people to feel offended".
HCRG chief nurse Sarah Wardle said: "We don't always get it right and for that I am sorry but I do know professionally and as an organisation we're really keen to listen to improve all of the time and we're really open to feedback and to changing how we work.
"(It's) really important to have a shared understanding with the patient and family about phrases and terms that they're comfortable with.
"We would never, ever, ever want people to feel offended we all share the same aim to provide the best possible experience and quality of care and working together with families is absolutely the best way of achieving that."
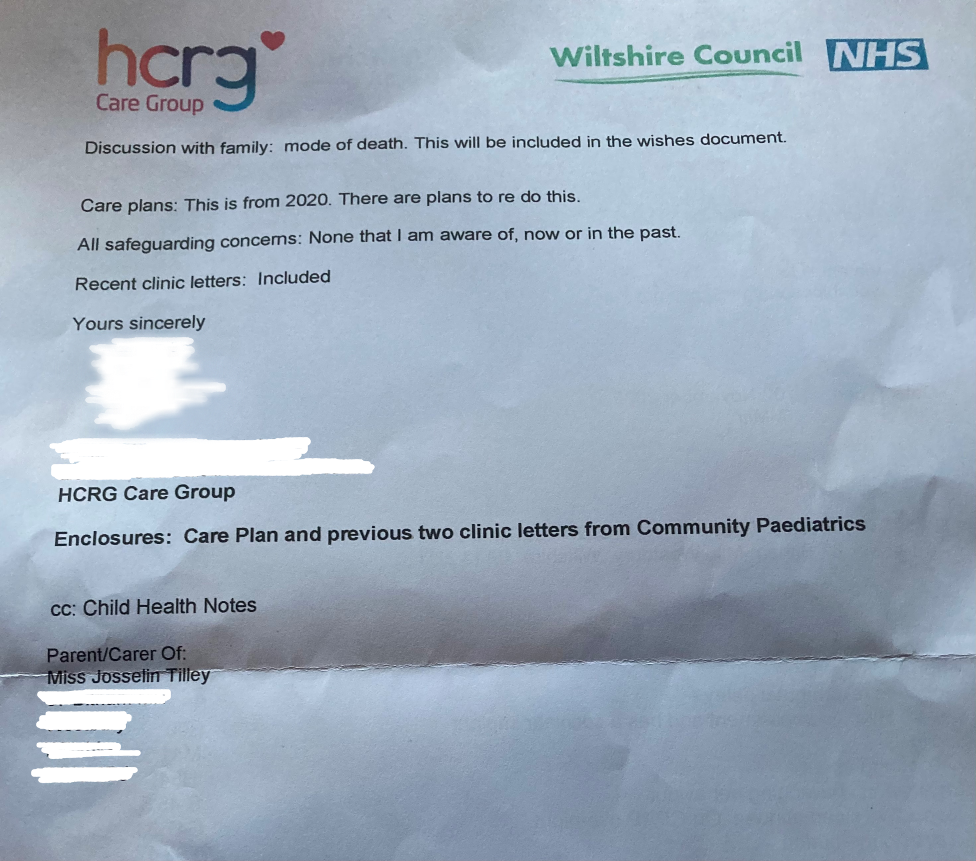
An extract of a medical letter received by Mrs Tilley shows the type of language used about patients in correspondence
Dr Fritz said that it is important that death is discussed with patients and those close to them: "For too long we have been afraid of discussing death and finding out what is important to patients.
"Conversations need to focus on a shared understanding of the patients' condition, of what is important to them, and what treatments they would or wouldn't benefit from.
"The Resuscitation Council UK leads on the ReSPECT process (Recommended Summary Plan for Emergency Care and Treatment, external) to help facilitate these conversations and ensure documentation that is acceptable to both patients and clinicians
She said that getting language right was a complicated issue, particularly around discussing death.
"Doctors are trying to gain a shared understanding with them patients about what the problems are and what to expect. We think we're doing a good job copying our patients into our letters to keep them informed, but the letters have to have really clear medical information for our colleagues.
"That's where the tension is because there is a technical language we use as doctors which can loose something in translation into lay terms - and, at worst, be upsetting for those reading it."
Doctor Fritz said the reason she and doctor Caitriona Cox were running the campaign, external at Cambridge University was because they recognised language regularly used by clinicians was often problematic for anyone outside of medical practice.
"Even just (the term) presenting [a] complaint. Patients coming into hospital with whatever's bothering them we [doctors] talk about as a complaint and I think that infantilises the patient. They're not complaining when telling us what's going on."
The team has invited patients and their families to share examples of problematic medical language they have encountered, and what form of words they would prefer medics to use instead, to help feed into the campaign.

Mrs Tilley says she finds the tone used to discuss her daughter's death upsetting

Follow BBC West on Facebook, external, Twitter, external and Instagram, external. Send your story ideas to: bristol@bbc.co.uk , external
Related topics
- Published22 November 2022

- Published16 November 2022
