Northern Ireland mental health targets not being met
- Published

The Health and Social Care Board says there is a "high risk" of continuing breaches of the 13-week waiting target without additional investment.
None of Northern Ireland's health trusts is meeting their waiting time targets for people with mental health problems like anxiety and depression.
According to the Health and Social Care Board, there is a "high risk" of continuing breaches of the 13-week target without additional investment.
The board estimates an additional 160 full-time staff are needed to meet the growing demand for treatment.
The health minister said a social care workforce strategy must be developed.
"We clearly need a workforce plan," she said, in response to the BBC investigation.
"It is one of the things I was very shocked about when I took up office - that we didn't have an over-arching workforce plan for the entire health and social care system.
"So we have shortages in staff right across not just in mental health.
"So the workforce strategy is key. We need to decide where we need the staff, what is the best training for staff and where they should be best placed."

The minister said a lack of work force planning was one of the things she was most shocked about when she took up office.
In a statement to the BBC, the board said it "acknowledged and apologised" for the "unacceptable waiting times for psychological therapies".
It said the rise in waiting times was due to "increased awareness of the important role that psychological therapies play in enabling mental health recovery" and also reflected "a "legacy of unmet need".
The board also said while it had tried up keep up with demand, current capacity was "unable to keep pace with need" and within this context it estimated "an additional £17m would be needed" across primary care, Children's Adult Health Care and Mental Health Services.

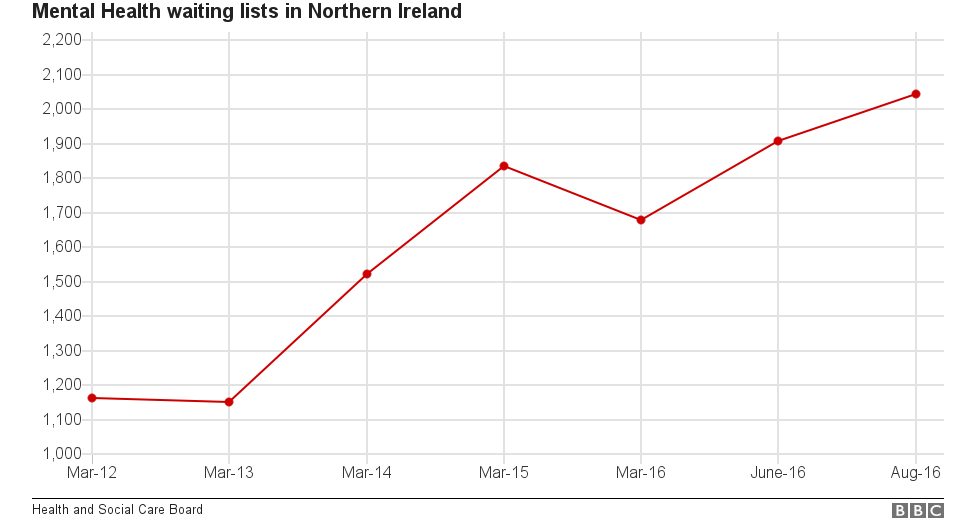
Figures from the Health and Social Care Board show there has been a steady rise in the numbers waiting for what are known as psychological therapies over the past five years.
That means people who need professional help from psychologists and psychiatrists for conditions which can include depression, post-traumatic stress and eating disorders.
The strategy on providing psychological therapies was set out by the Department of Health in 2010 because arrangements at the time were described as "extremely poor".
However, from the time it was established it was only partially funded.
Mental health figures in Northern Ireland
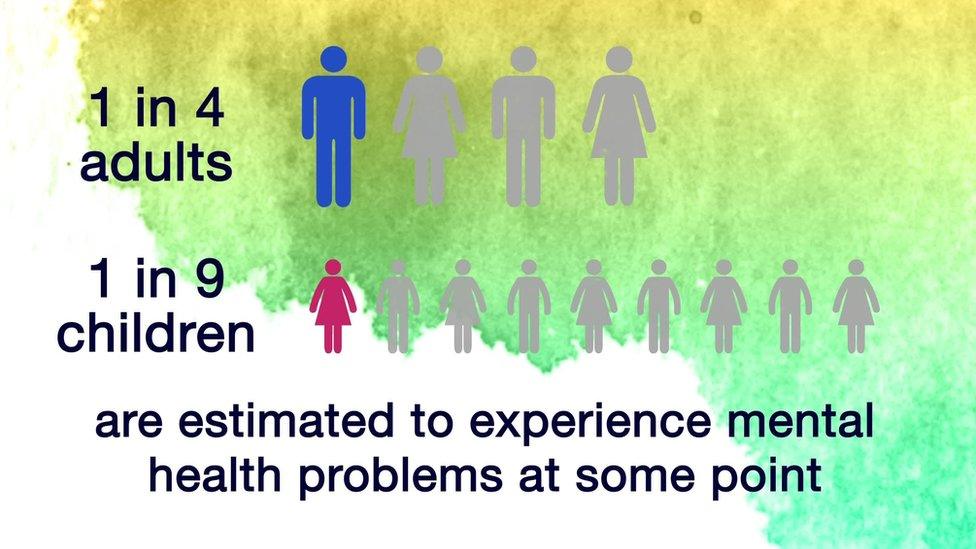
Northern Ireland's high levels of mental ill health are well known and are estimated to be 25% higher than those in the rest of the UK.
Research indicates that one in four adults will have mental health problems at some point and it is the single biggest cause of disability.
Despite this, according to the Health Board's own figures, external only 6% to 8% of their budget is spent on mental health and psychological therapy services.
Lord Nigel Crisp says mental health must be given the same level of priority as physical health
The current funding gap for psychological therapies in Northern Ireland is about £12m when compared to the rest of the UK.
These findings are supported by a recent review of psychiatric care in Northern Ireland conducted by the former chief executive of England's NHS, Lord Nigel Crisp.
"I think we were really surprised at the level of priority that was given to mental health, what's really important is to give the same level of priority of mental health as to physical health," Lord Crisp said.

Depression 'destroyed my family' - one man's story
No-one is immune from depression. A psychological disorder, it can grip anyone at just about any time.
While it cannot directly kill the same way that an illness like cancer or heart disease might, it can lead indirectly to a person losing their life.
Pedie McAllister knows all about it - his wife Joanne took her own life on 17 March 2015.
Read more here

"I think this isn't just about Northern Ireland - elsewhere in the UK and elsewhere in the world we haven't really got parity between the services.
"But there isn't even a policy of parity in Northern Ireland and the starting point is for your politicians to say 'we've got to do this, we've got to stop this' and make sure when somebody is severely mentally ill they get the same sort of service as they would expect if they had a heart attack or a stroke or something like that."
Meanwhile, according to the Public Health Agency there has been a 12% increase in the overall rate of people self-harming in Northern Ireland.
A study found that between 2012 and 2015 approximately 16,300 people turned up at emergency departments seeking treatment, often on more than one occasion.
- Published15 November 2016

- Published15 November 2016
