Hyponatraemia deaths: Mother furious over nursing decision
- Published
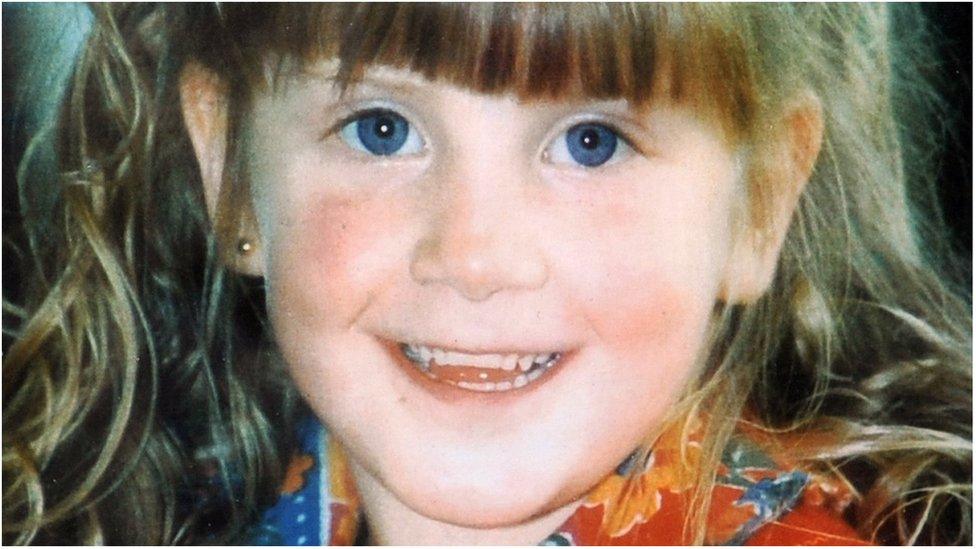
Nine-year-old Raychel Ferguson died in hospital in 2001
The mother of a child whose death in hospital was found to be avoidable has said she is furious no further action will be taken against nurses involved in her daughter's care.
The Nursing and Midwifery Council (NMC) told Marie Ferguson the failings identified have been addressed.
It said no further action was required at this time.
The Hyponatraemia Inquiry found four out of the five deaths it investigated were preventable.
Hyponatraemia is an abnormally low level of sodium in blood and can occur when fluids are given incorrectly.
The damning report was heavily critical of the "self-regulating and unmonitored" health service.
Raychel Ferguson was nine-years-old when she died at the Royal Belfast Hospital for sick Children (RBHSC) in June 2001, a day after an appendix operation at Altnagelvin Hospital, Londonderry.
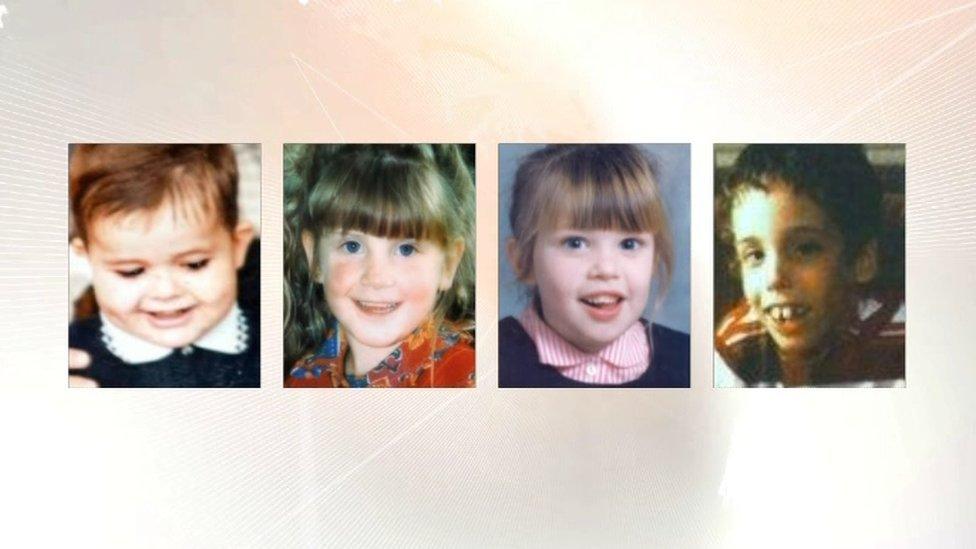
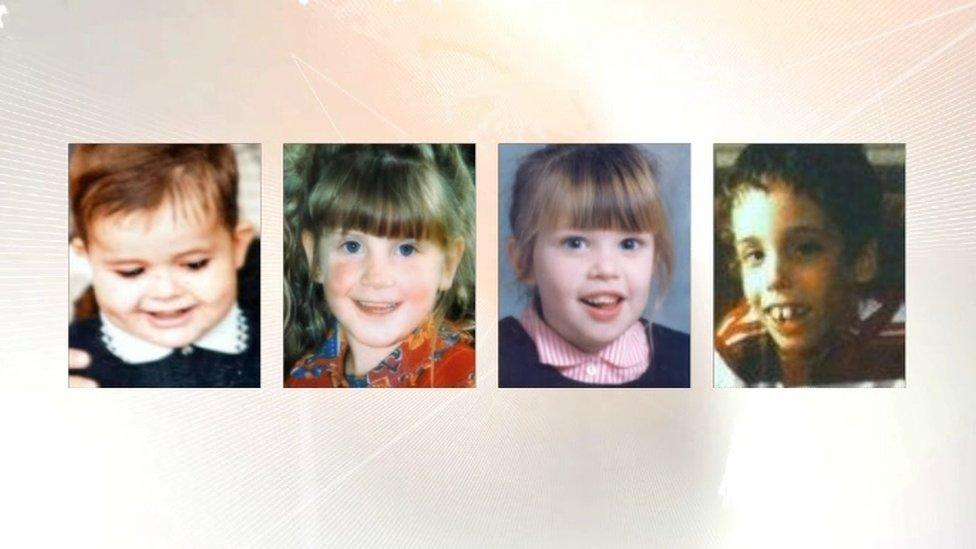
Four other children - Adam Strain, Claire Roberts, Lucy Crawford and Conor Mitchell - all died at the RBHSC between 1995 and 2003.
In a letter to Raychel's mother Marie Ferguson the NMC - the regulatory body for nurses - said that while the allegations were "extremely serious" they had "concluded that the failings identified have been addressed so there is no further action they could take at this time".
Mrs Ferguson said she was "extremely disappointed" and called on the NMC to reverse its decision.
'Not intended to punish'
In a statement to BBC News NI, an NMC spokesperson said: "It's clear that there were serious failings in care around hyponatraemia at Western Health and Social Care Trust and that these failings have had a devastating impact on the families involved.
"All of the nurses have undertaken training around recognising and managing hyponatraemia and the trust have made changes on the wards to assist with recognising and escalating concerns.
"We understand the impact of our decision on the family. We have been in contact with them and look to remain in contact with them throughout this difficult time."
Mr Justice O'Hara calls on medical professionals to put the public interest first.
The 14-year inquiry was chaired by Mr Justice O'Hara and his final report was scathing, both of how the families had been treated in the aftermath of the deaths and of medical professionals' attitude to his investigation.
He said some medical witnesses to the inquiry "had to have the truth dragged out of them".
Mr O'Hara's report made 96 recommendations - the first of which was that a statutory duty of candour be set up, breach of which would be a crime.
In a letter to Mrs Ferguson dated October 15th, the NMC said it took it seriously when nurses' actions have led to or contributed to death or serious injury.
BBC News NI Health Correspondent Marie-Louise Connolly explains the background to the hyponatraemia inquiry
But the NMC said its focus was on whether the nurse is likely to put patients at risk in the future, adding that the process is "not intended to punish nurses" and that they want to "encourage an open culture where patient safety concerned are reported."
The letter notes the evidence given by nurses to the public inquiry and that there was "no suggestion that the nurses were aware of the risks of hyponatraemia or had appreciated risks associated with Raychel's condition."
Therefore it was the NMC's view that "the nurses did not appear to knowingly take a risk with Raychel's condition."
'Devastating'
The NMC further outlined that it considered whether the conduct was likely to be repeated. In this case it said it had been informed by the Western Health and Social Care Trust that a number of measures had been taken to address the concerns raised by the inquiry.
It also stated that it had been told by the Western Trust that "all nurses have shown remorse and are insightful as to why the failings at the time contributed to Raychel's death."
Finally the decision letter states that sometimes regulatory action against a nurse may be needed "to promote and maintain public confidence, even when we don't think the nurse poses a future risk to patient safety."
The NMC letter states that it accepts that the failures in care in Raychel's case were very serious and the outcome "devastating".
However, it added: "The subsequent actions taken by the trust and the Department of Health have appropriately addressed the failings identified and because of this, it's not necessary for us to take further regulatory action to address these concerns."
In June the Department of Health established a number of workstreams to implement the recommendations of the public inquiry, such as establishing a duty of candour and an independent medical examiner.
- Published31 January 2018
- Published31 January 2018
- Published31 January 2018
- Published8 May 2018

- Published29 May 2018