Endometriosis: Women in NI 'not getting good deal'
- Published
"I was a stranger in my body"
Women in Northern Ireland are not getting a good deal from the health service, according to the head of the support charity Endometriosis UK.
Angela Style said women are living in limbo with challenging symptoms.
Waiting times for endometriosis treatment were "shocking", she said, with some women waiting two years for an appointment with a consultant.
The condition causes tissue similar to the womb's lining to grow elsewhere in the body, and can lead to infertility.
Department of Health figures show that the total number of women waiting for a gynaecology outpatient appointment has more than doubled in seven years.
A spokesperson on behalf of health and social care in Northern Ireland apologised, describing the waiting times as unacceptable.
Affecting women's lives
As part of BBC research, more than 380 women from Northern Ireland shared their experiences of endometriosis.
Nearly all of them said it had badly affected their mental health, career opportunities, sexual relationships and education.

Sarah McCann says she was told her pain was "normal" or a "woman's problem"
Most said it had badly affected their fertility and about half said it had led to suicidal thoughts.
The latest figures show the number of women waiting for a gynaecology outpatient appointment rose from 7,700 in 2012 to more than 17,000 in March.
Patients with endometriosis often need a procedure called laparoscopy or keyhole surgery, in which an incision is made in the abdomen and pelvis.
In 2010, 221 patients were waiting for a laparoscopy. By March, the number had almost tripled to 606.
Of those waiting, nearly half have been doing so for more than six months.

What is endometriosis?
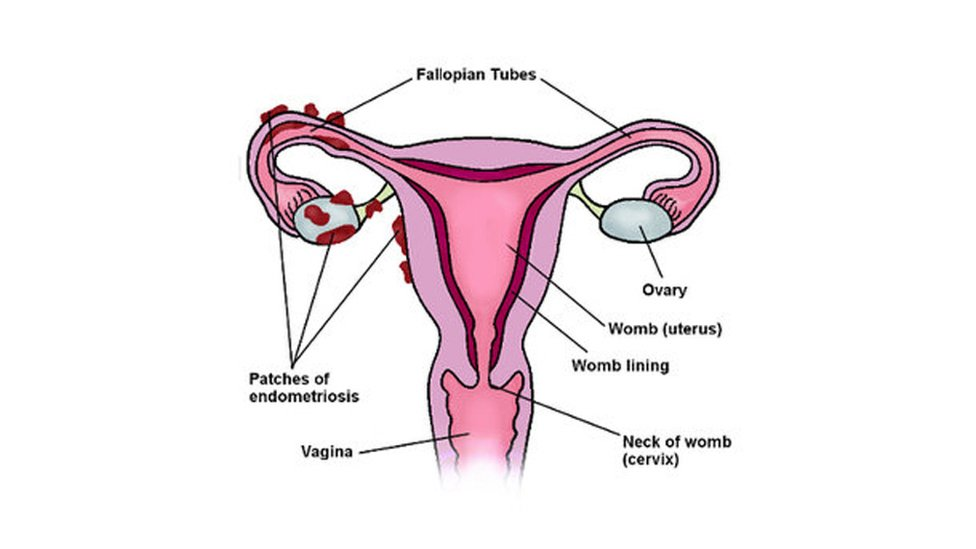
How endometriosis builds up around the fallopian tubes and ovaries
Endometriosis is a condition whereby tissue similar to the lining of the womb is found outside the womb, such as in the ovaries and fallopian tubes.
It mainly affects girls and women of childbearing age. It is less common in women who have been through the menopause.
It is a long-term condition that can have a significant effect on a woman's life, but there are treatments that can help.
Symptoms include pain in the lower tummy or back (pelvic pain), usually worse during periods; pain when going to the toilet during periods; feeling sick, constipation, diarrhoea or blood in urine during periods; difficulty getting pregnant.
For some women, endometriosis can have a big effect on their life and may lead to feelings of depression.

A Health and Social Care spokesperson said it was "regrettable that some patients have to wait longer than they should for assessment or treatment at a gynaecology clinic".
"However, waiting times across all specialities have been increasing since 2014 as a result of wider financial pressures."

The number of women waiting for an appointment has risen by almost 10,000 in seven years
Across the UK, women often have to wait a long time for diagnosis - the average is seven-and-a-half years.
Belfast woman Sarah McCann said she waited a decade to be told she has endometriosis, which happened after she paid for surgery privately in England this summer.
The 28-year-old said she does not just experience heavy periods but suffers constant chronic pain in her bladder, bowel, vagina and lower back as well as fatigue and nausea.
She said she struggled to get her physical pain addressed, having been told it was "normal" or a "woman's problem".
"It is a really serious thing and I think people really dismiss it," said Ms McCann.
"If someone had intervened when I was 18, I wouldn't have gone through the mental and physical anguish."
'At war with my body'
A Health and Social Care spokesperson said endometriosis can be difficult to diagnose because symptoms can vary between patients and over time.
"Sometimes several clinical specialities are involved in the investigation of one woman over time and this, in combination with waiting times, can indeed take years until a diagnosis is confirmed," they added.
Sarah McCann said the condition left her isolated, depressed and "at war" with her body.
"Mentally it's had a massive impact on me, I think really because of the not knowing," she said.
"There were many days when I felt suicidal, that I can't go on."
She said she felt her education, career and social life had suffered and her dreams of being a journalist had been shelved.
"You have to have sick days. I constantly feel like I'm not a good enough employee," said Ms McCann.
"I'm always going to be less than the other people out there."
New model for assessing condition
Now planning a future with her fiance, Sarah said she may consider returning to England to live because of the waiting times in Northern Ireland.
NICE, the non-departmental public body responsible for issuing advice on treatment, has guidelines stating that women should have access to a specialist centre if they have suspected or confirmed deep endometriosis involving the bowel, bladder or ureter.
The Health and Social Care Board has developed a Northern Ireland service model for the assessment and management of endometriosis.
That includes the recruitment of two endometriosis specialist nurses - one in Belfast and the other in the Western Health Trust.
In 2017, the Department of Health endorsed the NICE clinical guidance on the treatment and diagnosis of endometriosis.
Endometriosis UK has also called for Northern Ireland's education system to implement "age appropriate menstrual wellbeing", a measure that will be rolled out in England from 2020.
- Published26 November 2018

- Published7 August 2017
