Mumps: Northern Ireland cases 700% rise down to vaccine cycle
- Published
- comments
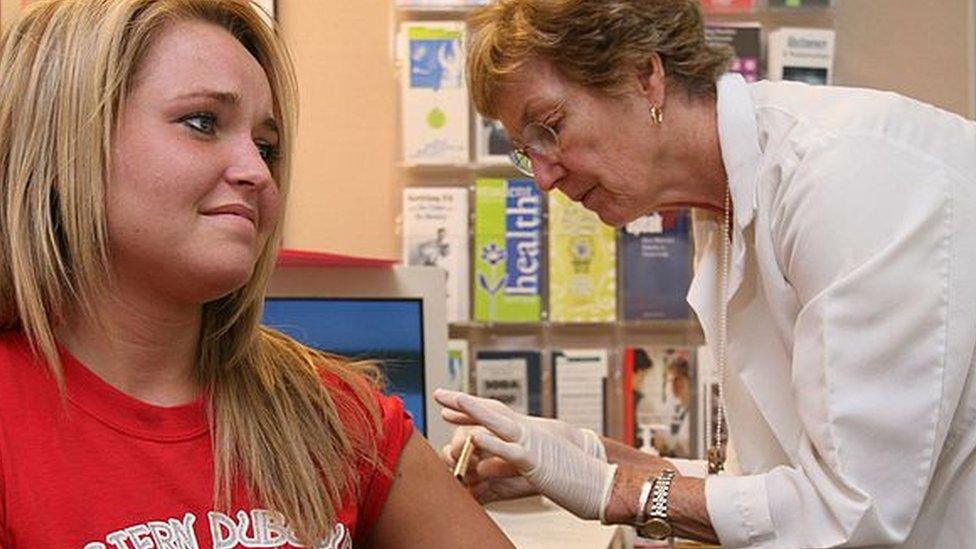
The MMR vaccine protects against measles, mumps and rubella
A 700% rise in cases of mumps in Northern Ireland is partly due to the vaccine becoming less effective over time, the Public Health Agency has said.
There were 534 confirmed cases last year, compared to just 67 in 2018.
Dr Jillian Johnson said the majority of the cases were people aged 15-24 who have had two doses of the MMR vaccine.
She said there is a rise in cases every two to three years as the mumps strand of the vaccine becomes less effective.
Dr Johnston said people who have had the MMR get a milder form of mumps.
Children are offered the MMR vaccine at 12 months and three years of age.

Dr Jillian Johnston said over time the mumps component of the MMR vaccine becomes less effective
"We expect to see a rise in mumps activity every two to three years and that's what we're seeing at the moment," Dr Johnston said.
"We know that the mumps component of the vaccine decreases and becomes less effective over time.
"So every two or three years the number of people who are susceptible to getting mumps increases and that's what's happening."
Dr Johnston said people who have not been vaccinated can suffer from serious complications from the virus, including swelling of the brain and meningitis.
She said of the 2019 cases, 23% had not had two doses of the MMR vaccine.
There have been 79 cases of mumps so far in 2020.
Dr Johnston said the figures show "a bit of a seasonal fluctuation".
"We would expect to see that trajectory and increase for the first six months of this year, then for the second half of the year we would expect to see a decline.
"We would like them to be lower and that's why we want people to make sure they have had two doses of MMR."
It has been revealed that cases of mumps in England reached their highest level in a decade.
Outbreaks in universities and colleges raised the number of cases of the painful viral illness to 5,042 in 2019 - four times the number in 2018.
Teenagers and young adults who have not had two doses of the MMR vaccine are deemed "particularly vulnerable".

Swollen glands below the ears are a classic sign of mumps
There were also increases in mumps cases in Wales and Scotland, external in 2019.
Dr Johnston said people could check if they have had two doses of the vaccine through their GP and that it was particularly important for people travelling to universities to do so.
She that the increase in Northern Ireland was not as severe as in England because there has traditionally been a better uptake of vaccinations and NI was not as badly affected by a scare over MMR that hit England in the 1990s.
"In the scare in the '90s there was a small effect from that, but it wasn't as marked as in England," she said.
"Now we're lucky, because whilst we're seeing the mumps activity higher this year, it's not as high as what England is experiencing because they were affected by the scare more than we were in Northern Ireland."
What is mumps?
It is a viral infection that used to be very common in children before the MMR (measles, mumps and rubella) vaccine was introduced in the UK in 1988.
A classic sign is puffy cheeks under the ears.
Mumps is contagious and spread through infected droplets of saliva breathed in through the mouth or nose.

What are the symptoms?
painful swelling of the glands at the side of the face
headache
fever
joint pain
feeling tired
loss of appetite
Most people usually recover without treatment.
But in rare cases, there can be serious complications, such as inflammation of the testicles in males, meningitis and deafness.
Source: NHS UK, external

Why do some people still get mumps?
The part of the triple vaccine that specifically protects against mumps is not quite as effective as the elements protecting against measles and rubella.
However, getting the jab is still crucial - because the more people who are protected, the less likely mumps will be shared around.
During outbreaks among students, which are common, completely unvaccinated people are at highest risk.
Even if you get the illness after being vaccinated, you are likely to have a less serious form of it and fewer complications.
Why do outbreaks happen?
Cases of mumps consistently outnumber measles and rubella cases every year.
Teenagers and young adults in colleges and universities are now the ones who tend to be affected - for several reasons.
The mumps virus is very contagious and can be passed through saliva or droplets
Many of the 2019 cases were born in the late 1990s and early 2000s and missed out on the MMR vaccine when they were children.
Research by a disgraced UK doctor, Dr Andrew Wakefield, falsely linking the vaccine to autism undoubtedly had an impact on uptake.
Current students may also be too old to have been immunised or offered the MMR, or may only have had one dose of the vaccine and thus not be fully protected.
It is also possible the vaccine's protection against mumps may have worn off.
- Published14 February 2020

- Published14 February 2020
