Coronavirus: The patients making way to keep hospitals clear
- Published

Nicola and Austin Rothwell, the Grant family and David Hall are adjusting to changes in their healthcare due to coronavirus
Coronavirus has had a wide impact on hospital services in Northern Ireland.
Healthcare resources have been redirected to treating infected patients with many other procedures and appointments cancelled.
But that has meant other people, who credit their lives to the NHS, accepting changes to their care.
Some of them have spoken to BBC News NI about adjusting to a reduction in service and support.

A SIMPLE GUIDE: How do I protect myself?
AVOIDING CONTACT: The rules on self-isolation and exercise
LOOK-UP TOOL: Check cases in your area
MAPS AND CHARTS: Visual guide to the outbreak


'How he survived coronavirus the first time is a miracle.'
When Ollie Grant survived an earlier strain of coronavirus as a newborn, his parents said it was "a miracle".
Ollie, now aged one, has incurable congenital heart disease, which makes him vulnerable to even minor illness.
After contracting a coronavirus - different to the one behind the current epidemic - he had a stroke and was airlifted to Birmingham hospital.
Ollie's parents said their son would not be alive without the NHS.
Now the are struggling to adapt to looking after him at home without their usual extensive NHS support.

Ollie Grant's family is missing weekly home care visits
Damien and Riona Grant, from Kilcoo, County Down, said physiotherapists, community nurses, speech and language and occupational therapists used to call weekly to their home to help care for Ollie.
They said that was no longer possible due to the risk of infection. Riona said it felt as if their "security network" had been taken away.
"You are never out of the woods with Ollie, but with all of the amazing support of the NHS we have learned to cope," she said.
"We miss the security of them coming to the house to look after him."
Riona urged people to continue to stay at home to support the NHS workers and protect children like Ollie.
"There is no cure for Ollie and if he was to catch it [Covid-19] he would not survive," she said.
Damien said they now "walked a tightrope" of assessing when it was worth the risk of bringing Ollie to hospital.
"We have to decide what is the greater risk when his oxygen levels are low - taking him to a doctor or trying to deal with it ourselves."
Damien said Ollie must attend his next hospital appointment in mid-April, which is categorised as urgent.
"The thought of bringing him to hospital, an area with a concentration of people who may be affected, is terrifying but we don't have a choice," he said.
A South Eastern Health Trust spokesperson confirmed there were not as many direct health care visits due to the virus, although telephone support was available.
Services were still available to respond to urgent and high risk issues or for families struggling to cope, the spokesperson added.

'Other mums are a lifeline'
Nicola Rothwell's son Austin, 12, was diagnosed with leukaemia in 2018.
Austin was in intensive care for three months and spent a year learning to walk again.
He now attends regular clinics at the Royal Victoria Hospital, Belfast, for maintenance cancer treatment.
Nicola, from Belfast, said the clinics were now done as remotely as possible, which was "stressful, scary but necessary".
She said they were now allocated a slot by text message and advised to wait in the car park until they received another message to come inside.
Austin's blood results are also delivered by text.

"I always had access to a consultant, which was reassuring, but now the only person Austin sees is the person who takes his blood. It's frightening for the children as well," said Nicola.
"I miss the support - talking to other mums in the waiting room can be a lifeline."
Nicola said she was always anxious attending clinics, but said it was now more frightening to take "an extremely vulnerable child into a hospital".
She said there had been a wider emotional toll on Austin as other support was scaled back due to the crisis.
He was devastated by the cancellation of a residential scheme at Daisy Lodge in Newcastle run by the Cancer Fund for Children, she said.
"The first residential helped him find his courage - it was the first in a long time I saw him be a 12-year-old boy again," she said.
"When we told him it couldn't happen he broke his heart."
Nicola said Daisy Lodge brought the children together virtually instead.
"To hear him laughing online with the rest of them at home was brilliant," she said.
"Families with children with cancer feel isolated enough, the pandemic is making it so much more difficult."

'It will happen when it happens'
David Hall was diagnosed with kidney cancer a week after his wedding in 2013.
He had six years of dialysis before having a double kidney transplant in February 2019.
David said the NHS had saved his life on more than one occasion and is now waiting for parathyroid surgery because of side effects of long-term kidney dialysis.
He said he had been advised his operation, which is classed as elective surgery, should be carried out "sooner rather than later".
But due to coronavirus, he said "there was uncertainty around whether it was going to happen and when".
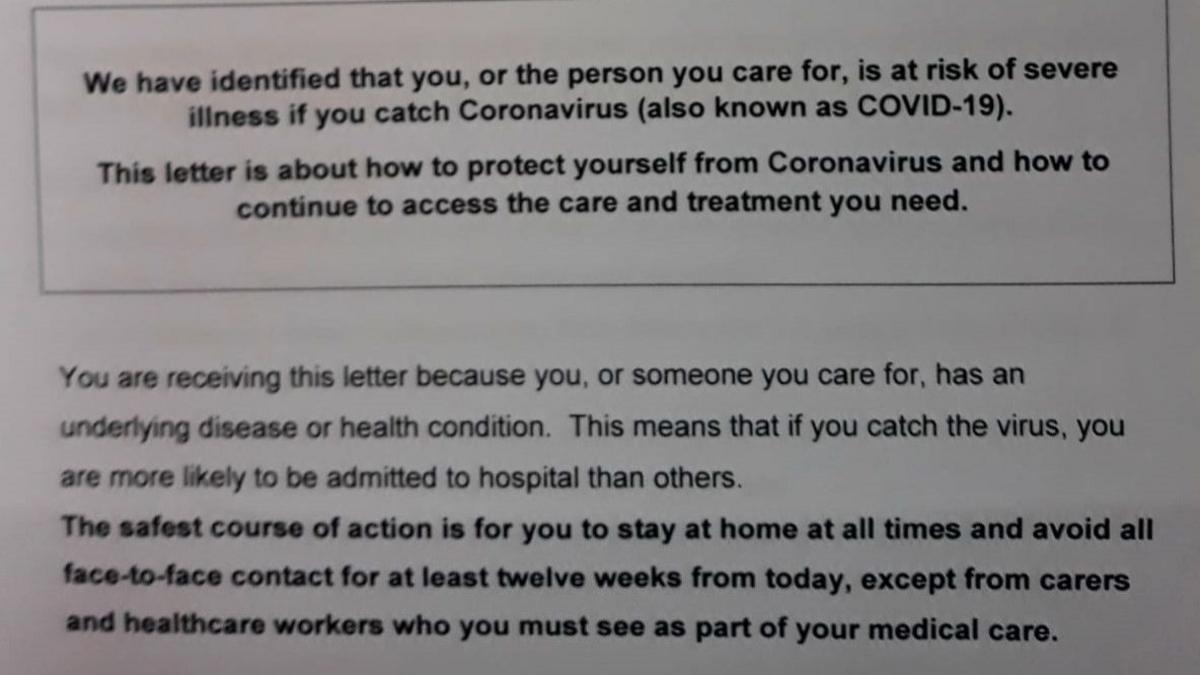
Forty thousand people in Northern Ireland have received letters advising them to stay at home for 12 weeks
David is one of 40,000 vulnerable patients in Northern Ireland who received letters from their doctors this week advising them to self-isolate for 12 weeks.
He said the main issues for waiting for surgery while waiting were "bone pain and potential fractures".
"An ongoing issue would be possible damage to the two transplanted kidneys - having two kidneys transplanted is rare," he added.
David said he had overcome so many hurdles since his diagnosis in 2013 that he was unperturbed by potential delays.
"There's no point in worrying about it, it will happen when it happens," he said.