Coronavirus: ICU staff 'exhausted and apprehensive' amid surge
- Published

Dr Leanne Davison from the BMA said Covid-19 is the biggest challenge in her 20-year career
As Northern Ireland's hospitals struggle to cope with the third, and possibly most deadly, surge of Covid-19, how are frontline health staff coping?
"I think the one word that would sum it up is exhaustion," said Dr Leanne Davison from the British Medical Association (BMA).
She told BBC News NI that 10 months into the pandemic, hospital staff were extremely tired and apprehensive that the worst is yet to come.
Dr Davison has worked in the intensive care unit (ICU) at Belfast's Royal Victoria Hospital for almost 20 years.
In that role, she is used to looking after Northern Ireland's most critically-ill patients, often having to deliver heartbreaking news to their families.
"There's not a week that goes by in intensive care without you having to have a difficult conversation - people don't come to critical care unless their life is at risk," she explained.
But she said the current Covid crisis has undoubtedly been the most challenging period of her career.
"I don't think any of us, when we started, could have anticipated the particular set of circumstances that we're facing now," Dr Davison added.
"There are more cases at present than there have ever been. We're quite concerned about some of the choices that we may be faced with."
As there is often a three-week lag between contracting Covid-19 and becoming seriously ill, many people who were exposed at Christmas are only now showing up in the hospital figures.
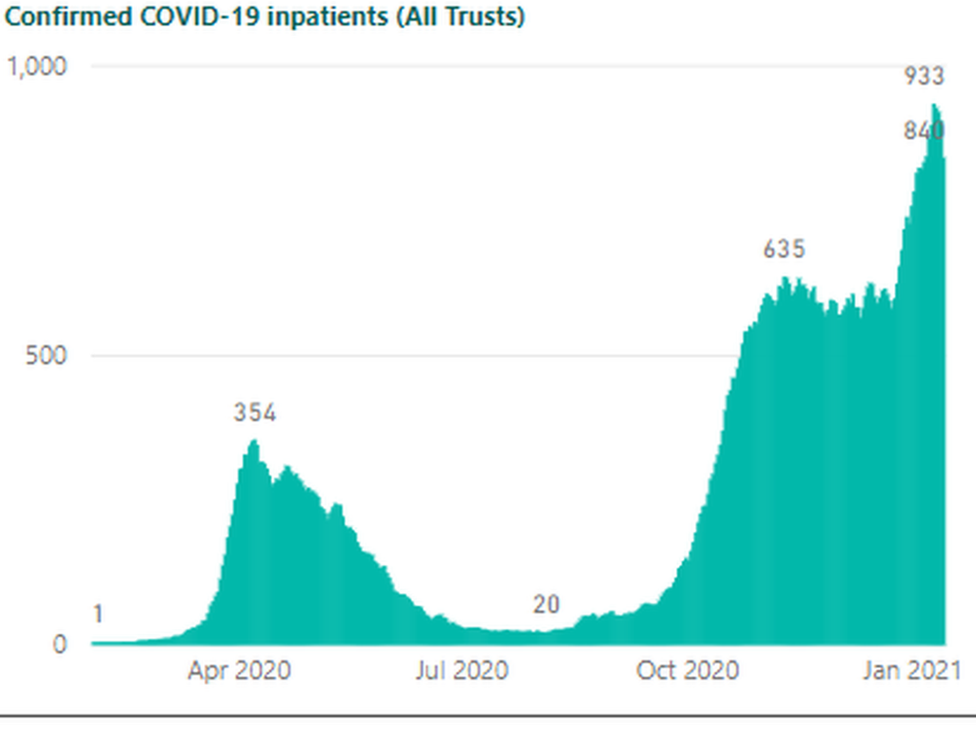
The past week saw the highest numbers of Covid-positive inpatients in Northern Ireland's hospitals since the pandemic began.
Daily hospital occupancy figures showed the number of patients with a confirmed diagnosis of the disease was in excess of 900 for most of last week.
"I think the overwhelming feeling at the minute is just exhaustion and apprehension," said Dr Davison, "because we know that the worst of it is to come yet."
"Obviously, none of us want to be in a situation where there's more patients than we can safely treat," she added.
"We want to do our absolute best for every patient and we're just concerned that, with the pressures that are placed upon us, we're not going to be able to provide the care that we would otherwise want to."
The relentless demand on hospitals is also far from ideal for frontline workers and their family lives.
Extra hours
At the start of the pandemic, the mother-of-two was moved to a 12-hour shift pattern - three days on and three days off.
"Not that I got any downtime on my three days off, because I have a 10-year-old and a 12-year-old. So on my days off I was home schooling," Dr Davison explained.
She hopes that the 12-hour shift rota will not have to return during this third surge, but adds she will "inevitably" end up working extra hours and weekends "just to get through the next six weeks".
Dr Davison is a member of the BMA's staff, associate specialist and specialty doctors committee

Currently, Belfast's most seriously ill Covid patients are mainly treated at the city's Nightingale and Mater hospitals but several still have to go to the Royal Victoria as it houses the regional trauma centre.
So if, for example, a car crash victim is brought in for emergency treatment, RVH staff must isolate them and wear full personal protective equipment (PPE) until the patient can be tested for Covid.
"We've had our fair share of working in PPE and gowns and difficult circumstances," Dr Davison said, but she expressed sympathy for colleagues who have to work all day in the full hot, uncomfortable PPE.
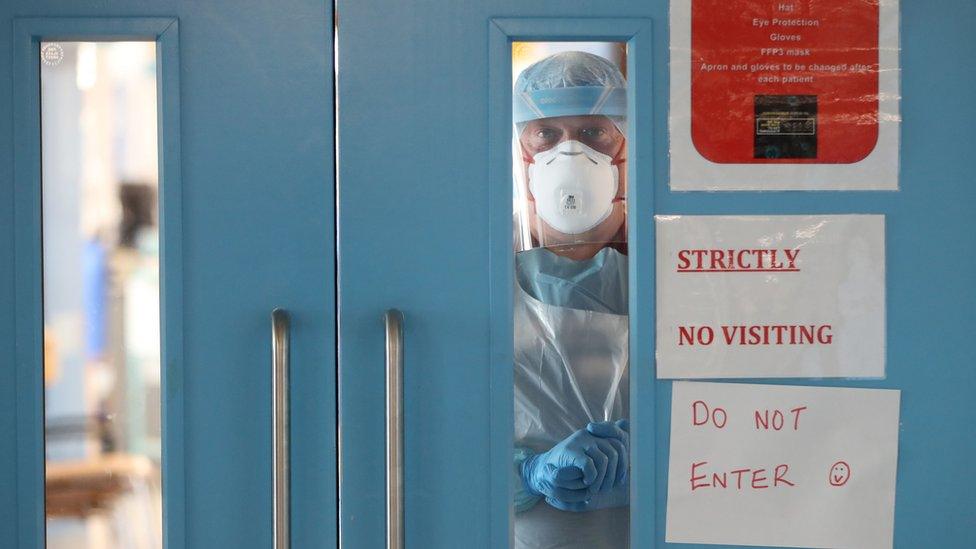
Strict hospital visiting restrictions were reintroduced last week due to rising Covid-19 infections
One of the toughest parts of any doctor's job is breaking bad news to patients' families, but that task has become even harder because of PPE and Covid restrictions on hospital visitors.
"While we've always supported families to visit at end of life, there are conversations that have to be had over the phone leading up that to prepare them," Dr Davison explains.
"It's very difficult when you're just talking on the phone and you can't see somebody's face, you don't have body language to guide whether somebody is taking in what you're saying."
Even when she is able talk to relatives face-to-face, she must now wear a mask which she said makes it much harder to show empathy and let families know "you are feeling for them".
Vaccine timings
Although Dr Davison has been on the frontline for 10 months, she has so far managed to avoid contracting Covid-19, but has concerns about how NHS staff are being protected.
Healthcare workers were among the first in line to be offered the Pfizer-BioNTech vaccine but the BMA representative said many of her colleagues disagree with the decision to delay the second dose.
Everyone will still receive their second dose, but this will now be within 12 weeks of their first instead of three weeks.
The US regulator and some UK experts have questioned the policy, saying it is premature without more trial evidence, but the UK's Medicines and Healthcare products Regulatory Agency (MHRA) says it is a pragmatic decision that will protect more people.
"Staff are worried that using the Pfizer vaccine like this will increase the risk of staff shortages at a time of crisis and also increase the risk of asymptomatic transmission," Dr Davison said.
She does agree however, that since the first wave, the health service has "learned a lot about how to treat Covid patients and how to manage our staff".
She pointed to the "quiet rooms" introduced in hospitals during the first wave and said the health trust is now providing psychologists to help staff who are struggling to cope.
"I think that we're very lucky in that we have a great team around us - particularly in ICU," she said.
"We're quite a close-knit community... we all get on very well and try to keep everybody's morale up.
"That sort of sense of team and family has kept us going through the worst of it."
Related topics
- Published15 January 2021

- Published15 January 2021

- Published14 January 2021
