Covid-19: 'I had my funeral planned in my head'
- Published

One of the CPAP machines is helping patient Gemma McQuoid breathe
It's tight, claustrophobic and at times unbearable.
But for some of the sickest coronavirus patients the CPAP (Continuous Positive Airway Pressure) machine is the last line of defence before a transfer to intensive care.
And for Sister Norma Kenny, who runs a respiratory ward at the Ulster Hospital in Dundonald, keeping people out of ICU is a priority.
"We have the experience to stay with the patient and to take away that fear factor of intensive care," she told BBC News NI.
"Once a person is told that they need to go to ICU they immediately think this is the end."
BBC News NI has been given exclusive access to Ward 3A at the Ulster Hospital - a 24-bed unit which has been operating at almost full capacity since the start of the pandemic.
'It's unbearable'
About 888 patients have been treated on the ward for coronavirus since April - 28 of them have had to go to ICU.
Sister Kenny added: "I would say 80 to 90% of our patients are going out of here beating the virus which is all down to good care but also down to the patient who fought that battle and worked with us to wear the CPAP machine."
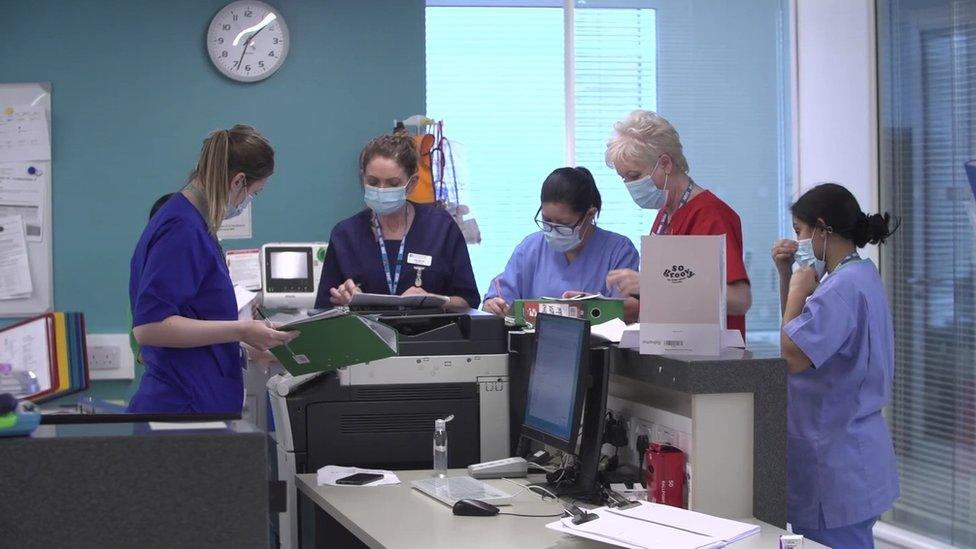
About 888 patients have been treated on Ward 3A since last April
CPAP machines allow people to stay conscious while oxygen is pumped into their lungs at high pressure to keep the airways open.
They can use up to 50 litres of oxygen per minute, per patient.
For Gemma McQuoid, whose oxygen plummeted to critically low levels in recent days, it has quite literally been a lifeline.
"It's a bit unbearable," she said, barely audible from behind the mask.
"You just pull through," she added.

Jacqueline Ogle has spent the past two weeks in Ward 3A
Meanwhile along the corridor in room 16, Jacqueline Ogle from Comber, County Down, was preparing to leave hospital.
The 62-year-old grandmother had spent the past two weeks in Ward 3A.
And while much of that time is a blur - the bedside discussions about a possible move to ICU - remain vivid.
'They have brought me back from the brink'
"I had my funeral planned in my head," she said.
"I felt this is the end; I haven't made it. And then I thought 'right Jacqui you have fight - they are going to help you'".
Ms Ogle, who works in financial services, spent many hours every day hooked up to the CPAP machine.
"They have brought me back from the brink," she added. "I was probably further down the line, closer to death than I will ever, ever realise."
"They brought me in and introduced me to the CPAP - a horrendous machine; I can see why people struggle with it. I can see why elderly people just can't even get it. It just seals your whole face.
"But I wore it all night."
According to the statisticians, the latest surge of the pandemic may have peaked in terms of new positive cases.
But hospital inpatient numbers remain stubbornly high.
And so the long, sterile corridor between Ward 3A to the intensive care unit is a familiar path trod by doctors and nurses who have seen a change in the patient profile.
According to Sister Kenny, more younger people who have no underlying conditions, 40s and 50s, and couples are now being admitted for treatment for Covid.

Dr Julia Courtney says as a result of people meeting up over Christmas many patients passed the virus on to other family members
It's also not unusual for several members of the same family to contract the virus.
Dr Julia Courtney: "They come in and are very scared, they are struggling, sick and have no idea of what to expect, they automatically think they are never going to get out.
"They also have regret that they have passed it on to other family members."
She added: "So there are huge, huge emotions that people are dealing with in a way that in normal life those emotions are not present.
"Sometimes we would have three members of the same family in different areas so sometimes you are going between A&E Ward 3A and intensive care to try and inform other patients of how their relatives are.
"And that was the effect of people meeting up over Christmas."
Related topics
- Published28 December 2020
- Published7 December 2020

- Published1 February 2021
