The EU healthcare option that ended with Brexit
- Published

The directive helped patients by refunding the costs of medical consultations and surgery
An EU healthcare option, no longer available in the UK due to Brexit, was growing in popularity on both sides of the Irish border, figures have shown.
The Cross-Border Healthcare Directive, external (CBHD) allows EU patients to arrange health treatment in most other European countries and claim back some costs.
Reimbursement is considered for both private and state-funded treatments.
More than £50m was spent reimbursing CBHD patients on both sides of the Irish border over the past five years.
It was particularly popular among cataract patients in the Republic of Ireland, about 2,000 of whom travelled to Belfast on so-called "cataracts buses" to have eye surgery in private clinics in recent years.
However, since the Brexit transition period ended on 31 December 2020, no new applications for help with costs for treatment after that date are being accepted from UK patients under the directive.
It means less choice for UK patients at a time when waiting lists are lengthening and NHS services, even urgent cancer surgeries, have been significantly curtailed by the pandemic.
However, critics of the EU scheme argued the NHS should not foot the bill for private healthcare abroad when it does not routinely offer to fund private treatment at home.
Brexit also means EU residents, including those in the Republic of Ireland, can no longer apply for UK-based healthcare through CBHD.
However, the Irish government has set up a temporary replacement scheme for its residents who seek treatment in Northern Ireland.
How many people used the scheme?
The EU Cross-Border Healthcare Directive was more popular in the Republic of Ireland than it was in Northern Ireland, according to figures obtained by BBC News NI.
Over the last five years, Ireland's Health Service Executive (HSE) processed almost 16,500 successful applications, reimbursing Irish patients at a total cost of €47m (£40m) for treatment outside the state.
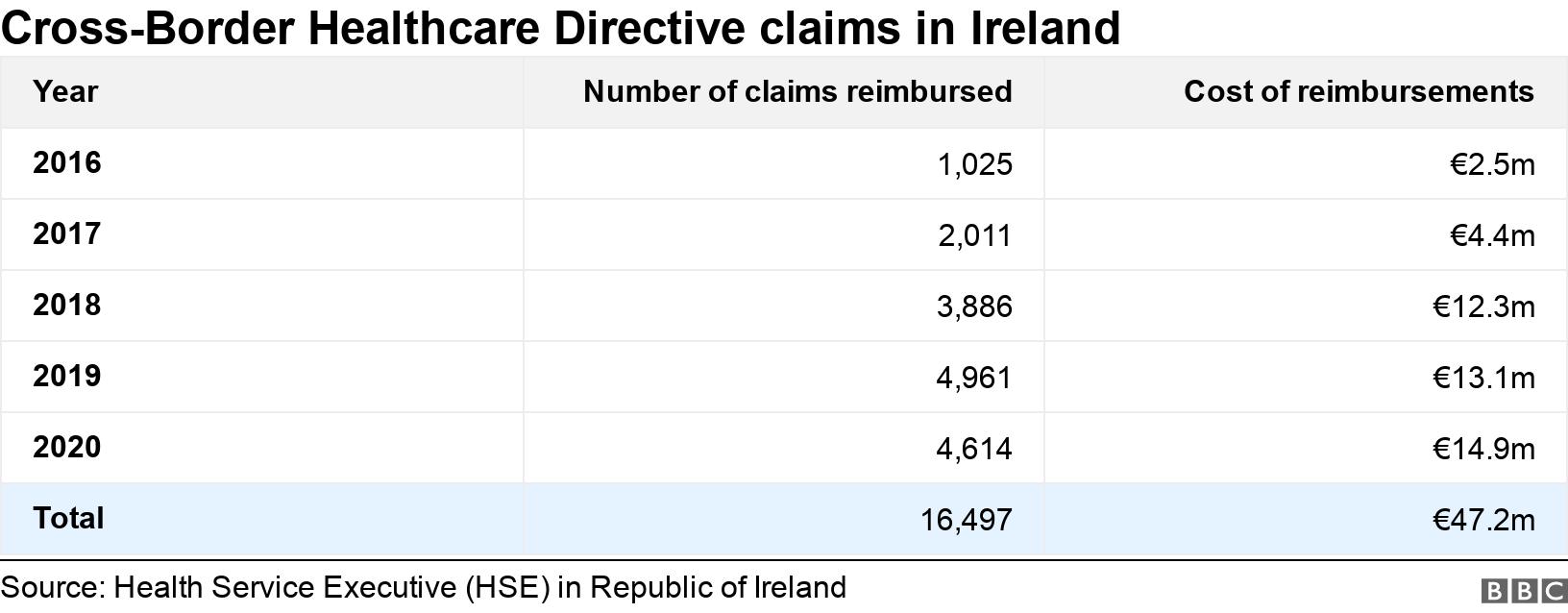

The bill was paid by Irish taxpayers as CBHD costs are met by the applicant's home country.
A further breakdown of figures shows that when Irish patients sought prior approval for UK healthcare under CBHD in the last five years, 97% of requested treatments were in Northern Ireland.
'Belfast or Blind'
About two years ago, Cork politician Michael Collins began organising buses to Belfast so patients from the Republic could get cataract surgery and claim back costs under CBHD.
He told BBC News NI some of his passengers faced five-year waits for surgery in the Republic and several were at risk of losing their sight.
Mr Collins set up "Belfast or Blind" bus trips with fellow parliamentarian Danny Healy-Rae and together they organised about 65 cataract coach trips to Belfast clinics.

Cork politician Michael Collins (centre) says the Belfast coaches were dubbed the Cataracts Express
Patients who did not have the money to pay upfront were assisted in getting credit union loans, on the assumption they could repay through CBHD refunds.
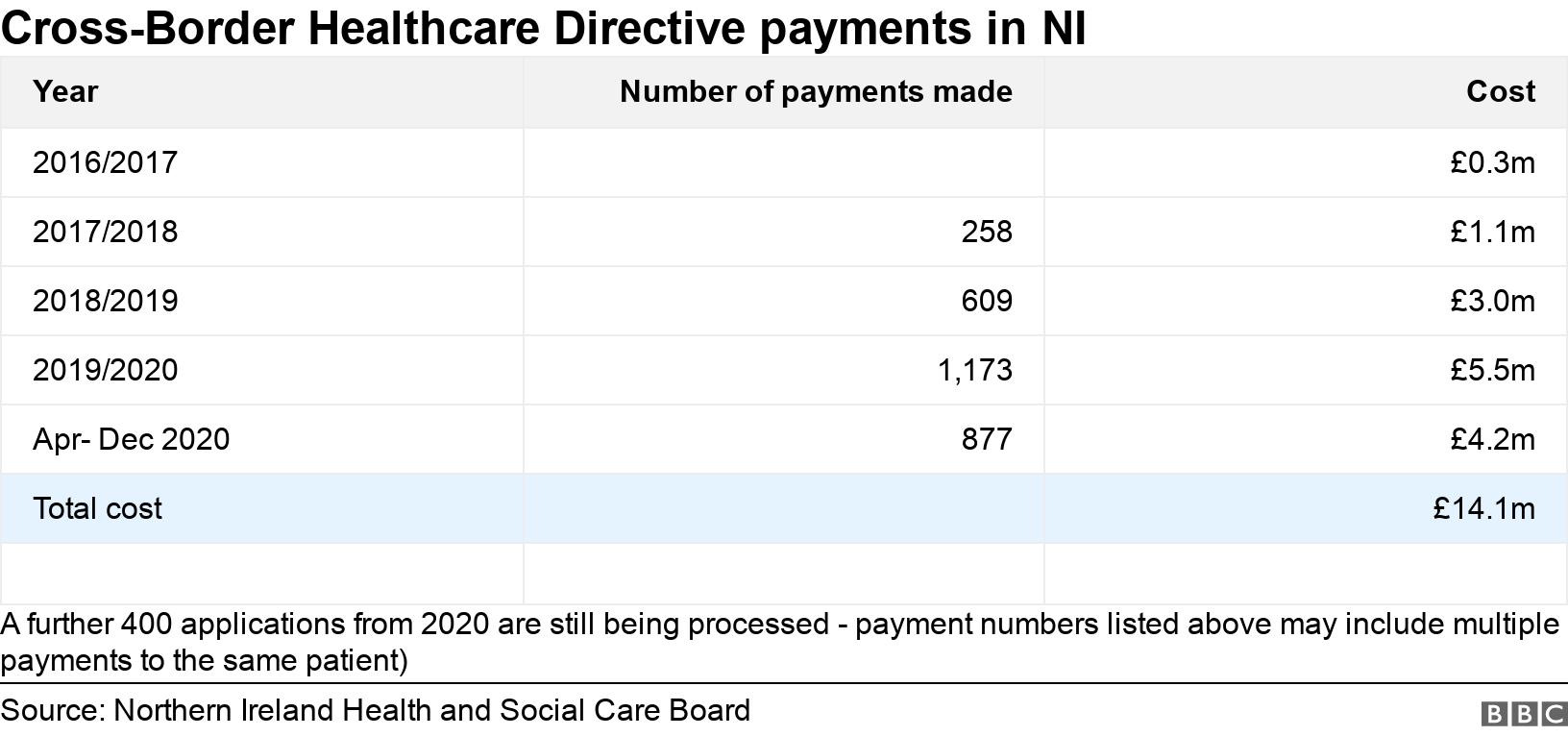
In Northern Ireland, the Health and Social Care Board processed substantially fewer CBHD applications over the past few years than their southern counterparts.
But it still spent a total of £14m reimbursing Northern Ireland patients for CBHD treatments in EU states between April 2016 and 31 December 2020.

What happened after the Brexit transition period?
The EU directive "no longer applies to all UK patients and was closed on 1 January 2021" according to Northern Ireland's Health and Social Care Board (HSCB).
"The board is not aware of UK and EU arrangements to replace the scheme," it told BBC News NI.
The HSCB pointed out that under the recent Brexit trade deal, it still considers requests from NHS patients to fund healthcare in European countries, albeit through different routes.
But unlike under the EU directive, UK patients no longer have the option of choosing private healthcare in an EU state, paying upfront for treatment and seeking refunds.
The destination country is also not obliged to give UK patients access to its state-funded elective treatments, and if there is a public health waiting list, UK applicants must join the queue.
Can Irish patients still cross the border for elective treatment?

Cataracts usually get worse over time without surgical intervention
Yes, for some services, because on 1 January 2021 the Irish government introduced a new "unilateral" arrangement for its own residents known as the Northern Ireland Planned Healthcare Scheme, external.
This allows patients from the Republic of Ireland to continue to access certain private healthcare treatments in Northern Ireland and apply for reimbursement from the Irish state.
Mr Collins is planning to restart his Belfast or Blind buses under the new scheme as soon as possible, when the Republic emerges from its highest level of Covid-19 lockdown.
However, as the new scheme is set to last only 12 months, Mr Collins wants a "longer-term solution" for patients on both sides of the border.
How does the Cross-Border Healthcare Directive work?
The EU introduced the CBHD in 2011 and the scheme still operates in EU member states.
Under the rules, EU citizens have the right to seek pre-arranged medical treatment in another EU state and ask their home country to cover the treatment costs.
A key requirement is that the treatment must be available in the applicant's home country through state-funded public healthcare.
Significantly though, applicants can choose either a public or private healthcare provider when they travel for treatment.
Reimbursement is based on the amount it would cost your own country's public health service to provide you with the same treatment at home, so it does not include travel expenses.
Additionally, not all treatment costs may be covered, so patients are advised to contact their own health authorities for advice before travelling.
Prior approval is not always necessary, but it can be a requirement if a particular treatment is "cost-intensive" or involves an overnight stay in hospital.
How do patients access healthcare outside NI after Brexit?

NI patients can still travel for health treatment but have less personal control over the arrangements
There are still two ways in which NHS patients can receive planned medical treatment outside Northern Ireland.
The first is known as the S2 (or E112) route, external which is available under the terms of the recent Brexit trade deal - the Trade and Cooperation Agreement.
Under S2 arrangements, Northern Ireland patients can submit their own requests for public health treatment in any of the 27 EU member states, particularly if there is a long waiting list at home.
However, this route can only be used if the treatment is already available through state-funded healthcare in both the UK and the country the patient wants to travel to.
S2 applications also require written support from a Northern Ireland consultant and prior approval from the Health and Social Care Board (HSCB).
The second pathway is known as Extra Contractual Referral (ECR), external - this happens when a consultant recommends transferring a patient outside Northern Ireland because the care they need is unavailable through local NHS services.
ECRs usually involve people who need specialist treatment in Great Britain, but they can be sent abroad in some circumstances.
However, patients cannot arrange care themselves - ECRs must be deemed "clinically necessary" by a consultant and require HSCB approval.
Why did the UK close CBHD to new patients?

NI is "disproportionally impacted" by the CBHD due to the Irish land border, Parliament was told
The EU directive is a reciprocal arrangement which no longer applied to the UK when the Brexit transition period expired.
In 2019, the UK's Department of Health laid out reasons to Parliament on why the scheme should be scrapped after Brexit.
In a legislative memo, external, it said: "It is odd to operate this scheme when it is not possible for UK patients to obtain reimbursement for private healthcare purchases within the UK."
It added there was "also a risk of inequalities as patients with financial means to access treatments abroad may be treated more quickly than otherwise and get reimbursement from the NHS, whilst less well-off, vulnerable patients cannot do so".
The UK department also pointed out that when it came to accessing cross-border healthcare, Northern Ireland was "disproportionally impacted due to the land border with the Republic of Ireland".
It said the EU directive "already creates severe pressures" on the UK Department of Health's budget and warned: "Any further financial exposure would again fall to DoH NI."
Related topics
- Published3 February 2021
