GP's 'distress' as patients complain about access
- Published
As patients complain over GP access. a Belfast doctor says their workload is "endless".
The perception that patients have lost confidence in the healthcare system is "distressing", a Belfast GP has said.
Dr Ursula Brennan, from Mount Oriel Medical Practice, was responding to criticism from some people about access to GPs across Northern Ireland.
She told BBC News NI their work throughout the pandemic had been "endless", "exhausting" and continued to be unrelenting.
Dr Brennan said GPs are there for their patients' needs.
While the experienced doctor accepted that dealing with patients over the telephone may have created an impression that GPs are not available - that is far from the reality.
"It is distressing for us that there is a perception that patients have lost confidence in us and our practice teams," she told BBC News NI.
"We have been working consistently throughout the pandemic covering our surgeries, providing vaccinations and working in Covid centres.
"The work has been endless."
Exhausted team
Dr Brennan's busy practice on the Saintfield Road has 7,500 patients on its books and just two full-time and three part-time GPs.

About 7,500 patients are registered with the Mount Oriel Medical Practice GP
Covid-19 meant they had to change "overnight" to continue providing a "safe and effective service for patients and staff".
The team, including receptionists, nurses and practice managers, have been left "exhausted".
Dr Brennan said the current "blended model" where a phone-first system is used, is likely to stay because "it's more efficient and for patients too".
BBC cameras spent a Monday morning at the surgery.
When the shutters went up at 08:30 BST the phones started ringing and they did not stop.
Social distancing meant there were just four people answering calls.
But the constant flashing red light showing the on-hold queue suggested a need for more.
They received more than 300 calls between 08:30 and 15:00 that day.
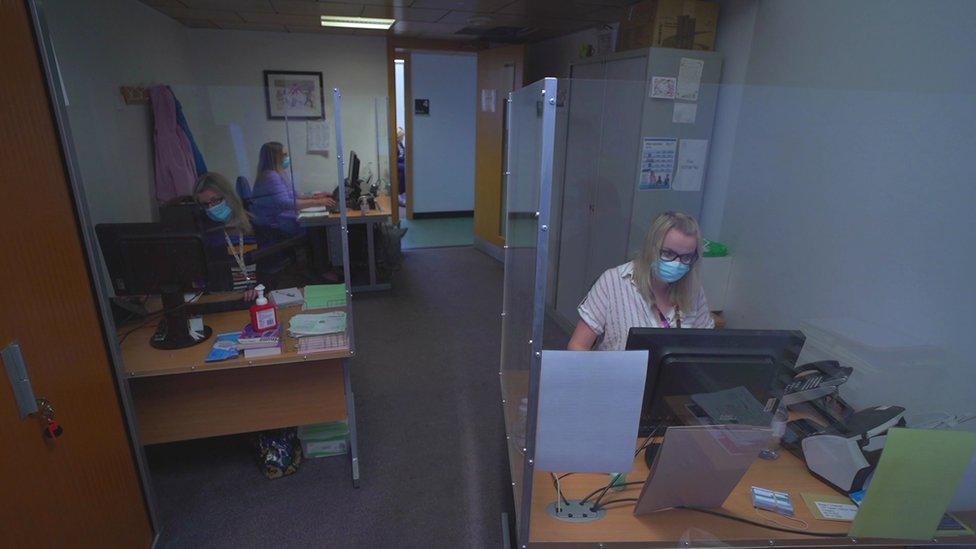
A small team of people handle hundreds of calls a day
Some 126 patients were offered a call-back with a doctor while six face-to-face appointments were also arranged.
There were also 40 nurse appointments in surgery with a further 90 phone calls made by staff about prescriptions, sickness certificates, lab results and enquiries about hospital waiting lists.
It was just a snapshot inside one of the 323 GP surgeries across Northern Ireland.
'We are doing more now than ever'
At the helm in Mount Oriel was practice manager Roberta Walsh, who keeps the practice up and running - ensuring telephones, IT, pharmacy, nurses and the GPs are all working.
There is the added workload of sourcing and maintaining personal protective equipment (PPE) as well as ensuring the vaccination programme runs smoothly.
GPs have delivered 671,000 Covid-19 vaccines in recent months - on top of thousands of other vaccines including for flu.
"We do things differently now people phone in and we arrange a call back with the GP then if a GP thinks they should be brought into surgery they will be given a face-to-face appointment, usually that same day," she said.
"It is definitely a more efficient way of doing things. Social distancing has made work life harder.
"There can only be a certain number in a room, space is tight we have to stay safe and ensure patient safety too.
"But I can guarantee you we are doing more now than ever."

Practice Manager Roberta Walsh says teams are doing "more than ever"
It might be a more efficient way of doing things but is it meeting patient's needs, as many people prefer that personal face-to-face contact?
Earlier this month the British Medical Association's Dr Alan Stout responded to criticism on social media from a small number of politicians who claimed some members of the public were not getting access to their GP.
It triggered a massive response from GPs across Northern Ireland who said they had been "flat out" during the pandemic.
But there were also numerous complaints from the public about unanswered phone calls, having to wait weeks to get an appointment and the lack of face-to-face contact with a health professional.
Dr Stout said the new phone-first triage model was more beneficial for the public and was a model that would mean primary care is "fit for the future".
"Funding is important and we are supporting the health minister's call for multiyear budgets so we can plan ahead not just for this year but for several years ahead so we aren't stopping and starting the system," he added.
The pandemic has shone a light on a system that's been fractured for more than a decade.
According to Dr Stout it took the pandemic to make change happen.
"It really pushed that change," he said.
"The pandemic has shown two things -that the system can change so quickly when we put our mind to it. But it has also shown all of the old creaks and gaps in the service.
"What we have got to do now is to look at the good and where the issues and gaps are and make sure that we then fill in those gaps and make sure that we have a sustainable service."
- Published20 May 2021

- Published19 May 2021

- Published19 June 2020
