Hospital beds 'at a premium' as NI emergency departments struggle
- Published
- comments
Senior nurse Jenny Nicholson says it is heartbreaking to see patients in A&E waiting so long for a bed
A senior doctor has warned that when people are being treated for more than 10 hours in ambulances, it means that emergency departments are "effectively closed for some of those patients".
Andrew Dobbin, a consultant at the Ulster Hospital, said the stream of very sick patients turning up at the emergency department was "relentless".
He said hospital beds were "at a premium".
Staff pleaded with the public to behave responsibly and "save Christmas".
Dr Andrew Dobbin says emergency services across Northern Ireland are overwhelmed
BBC News NI spent six hours in the Ulster Hospital's emergency department this week.
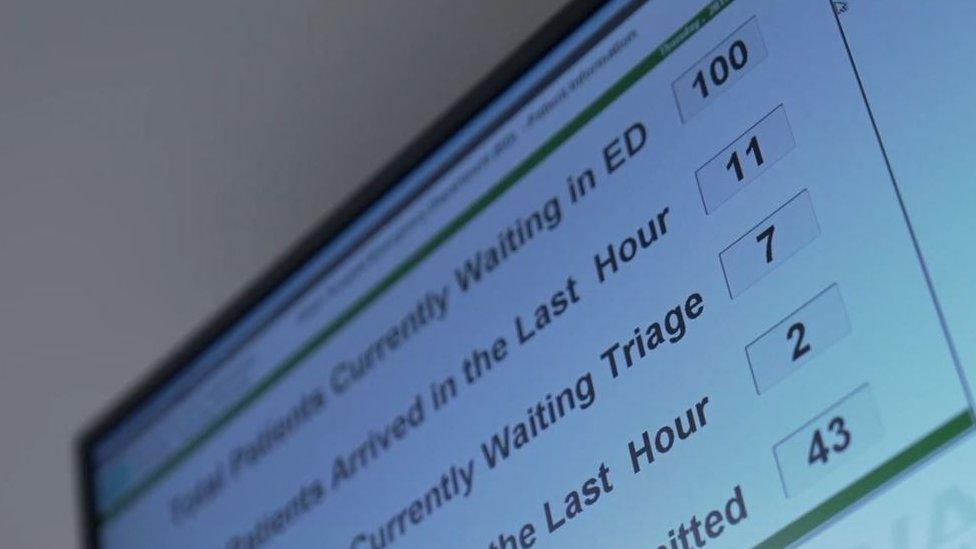
The numbers fluctuate but on Monday evening, at its peak, 134 people were there, including children.
Of those, 50 needed to be admitted to a ward. The problem was finding beds.
To allow new patients in, staff have to get people out of the hospital and back into the community.
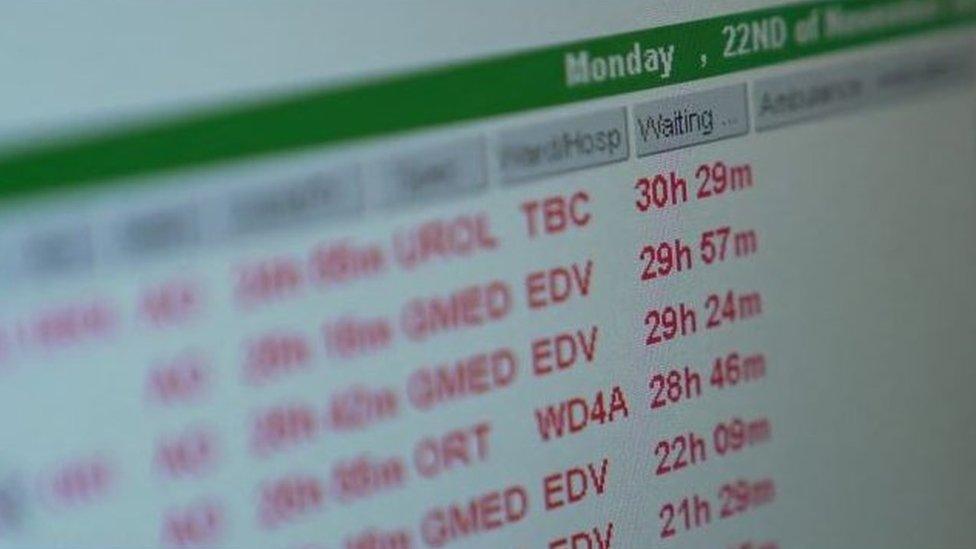
On Monday evening, at its peak, 134 people were at the Ulster hospital's emergency department
Marc Neil, the assistant director of unscheduled care at the South Eastern Health and Social Care Trust, allocates beds for people in hospital as well as in the community.
"Every day is a continuous struggle to find enough beds for everyone who needs one," he said.
"Every hour of the day that we move a patient is a choice to put someone there and someone not. Trained professionals are making those choices but, yes, it is tough."
Each health trust is faced with a similar problem.
On Monday night, more than 100 beds had been located in the community for hospital patients to be moved on.
But they were all declined because families said they were unsuitable for reasons such as where they were located or what facilities were offered.

Beds are being declined in the community as they aren't close to patients' homes or within their health trust
Mr Neil said "difficult conversations" had to take place but, he added: "We would remind people that the conversation we are having with you is the same conversation that we had with the person who was in this bed before you.
"At the moment, there are 103 beds available in the community but we can't get people to move out of hospital and into those beds as they aren't close to their homes or within their health trust.
"We are pleading with the public to work with us."

At the ED: Weary staff, patients waiting - and no end in sight
The nurses move around, fixing blankets and pulling curtains to protect patient dignity.
At every turn, there is a sick person waiting to be seen or to be admitted onto a ward.
At the peak, 134 people were waiting - in a department that originally housed 65 bedded cubicles.
Due to Covid, there are now several separate areas under one roof.
The Ulster Hospital emergency department originally housed 65-bedded cubicles but had 134 people waiting
Some patients sit in proper waiting areas - others are in corridors with babies wrapped in blankets on their laps, while others lie on trolley beds.
Older women peer out from under clutched blankets; younger patients scroll their phones.
Patients sit socially distanced alongside each other as staff scurry about delivering medication, applying IV drips and taking temperatures.
Every available space has been transformed into an additional waiting area - and everyone just seems to be waiting.
It is overwhelming to watch.

'Expect things to get worse'
When we spoke to him, Dr Dobbin had worked eight consecutive shifts, including with the Air Ambulance.
He said emergency departments across Northern Ireland were "overwhelmed".
"We are delivering care but perhaps not in the space where we want to deliver it - I expect things to get continually worse over the winter months," he added.
Things are precarious across the entire health and social care system.
According to the health trusts' winter plans, even if things were to stand still over the next couple of months - something that is highly unlikely - an additional 500 beds could be needed.
Dr Dobbin said the figure of 500 was becoming "a likely number".
"Right now, in November, there are 220 patients in emergency departments that are waiting for a hospital bed - we need those hospital beds right now.
"So considering how things might escalate with Covid and the winter pressures that number of 500 is looking likely."

According to the health trusts' winter plans an additional 500 beds could be needed
One patient described the number of people coming in and out as "mad" and said she had been waiting so long she had seen three different shift changes.
"Staff are great, I have to give it to them - I sat here all last night with no sleep... looks like I will be here tonight again," she said.
Lead emergency department nurse Jenny Nicholson said it was upsetting to see patients remaining in the department for several days.
"It's heartbreaking to leave them here in the ED knowing you are going to come back the next morning to see them again here," she said.

Jenny Nicholson says their focus remains on seeing patients as quickly as possible
"While we are providing the care that they need, the plan is in place and we are following that plan, they are not in the bed where they should be, where they would get the right care from a specialist."
Director of hospital services David Robinson said that the sheer numbers of patients was having knock-on effects on the rest of the hospital - including on surgery.
"Some of our sickest patients require to be cared for in intensive care, so with every additional bed we've put up in intensive care, regrettably we have to close a theatre for that week, which means unfortunately, we have cancelled operations."
He appealed for everyone to get vaccinated and said that many of the Covid patients who were in the intensive care unit had not been.

David Robinson has urged people to get vaccinated
"Just think about Christmas - it's for themselves, it's for their family, their neighbours but also for strangers - people they'll never meet, because for them, being in ICU means that surgery, unfortunately, has to be downturned."
Covid and the pressures of dealing with it remain constant - just one corridor away from the general emergency department is a ward where people with the virus are treated.
The same doctors and nurses attend to them, pulling on additional items of personal protective equipment (PPE) as they move from one area to another, with a sense of organised calm.
Related topics
- Published24 November 2021

- Published1 November 2021

- Published25 October 2021

- Published29 October 2021

- Published6 July 2021

- Published14 October 2021

- Published17 December 2020

- Published30 August 2021
