Health service: Northern Ireland 'short of almost 300 consultants'
- Published
- comments

Many health staff feel exhausted after two years of intense work during the pandemic, says the BMA
There were almost 300 consultant vacancies across Northern Ireland's five health trusts last year, according to analysis from the British Medical Association (BMA).
A report published by the organisation found there were 291 posts not filled by a permanent consultant in 2021, external.
The Department of Health's vacancy data for the same period showed there were 126 consultant vacancies.
The BMA in Northern Ireland said its analysis was more accurate.
The head of its consultants committee, Dr David Farren, said the department's data was based on the number of vacancies actively being recruited for.
"We have about 270 consultants missing from the workforce in Northern Ireland, which means the remaining workforce has to work harder," he said.
"They are exhausted.
"They are burnt-out from having worked so intensely over the past two years and a lot of them are now looking at retirement and saying: 'That is what I should be doing, going away a bit earlier.'"

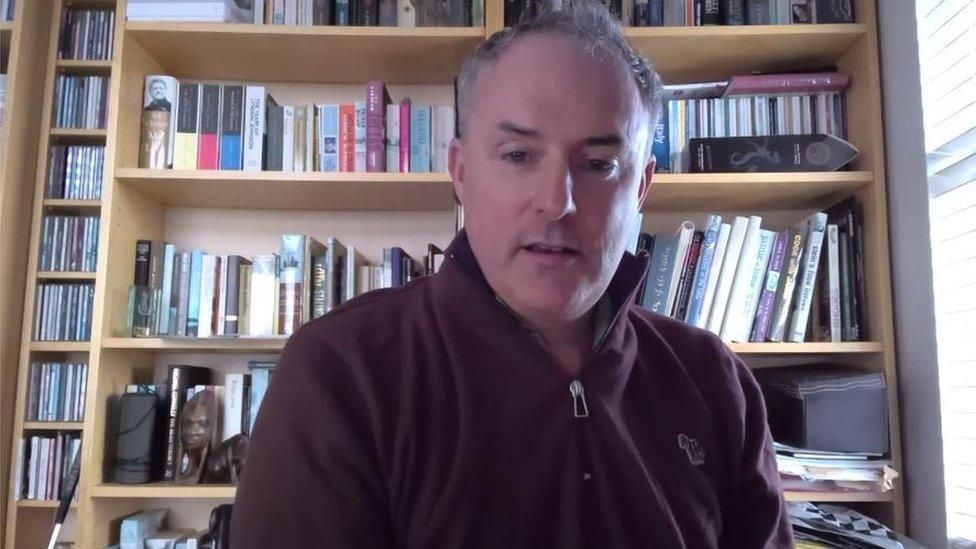
The BMA's Dr David Farren says a failure to plan has led to a shortage of consultants
Dr Farren said a failure to "properly plan" had led to a shortage of consultants along with a different rate of pay compared to elsewhere in the UK.
"A consultant will earn considerably less here, so it's very difficult to recruit people from the rest of the UK or bring people in from overseas and all of these things have come together now at a time when the workforce is overly stressed," he added.
A decision to remove emergency surgery from Daisy Hill hospital was taken by the Southern Health Trust last month, as it could not recruit enough consultant surgeons in Newry.
Health Minister Robin Swann has said a number of hospitals in Northern Ireland face an "ongoing challenge" in recruiting and retaining specialist clinicians, particularly those on smaller sites.
The Northern Health Trust recently launched a social media recruitment campaign for four consultant posts at the Causeway hospital in Coleraine, selling the benefits of living on the north coast.
A previous campaign saw the trust fill five vacant consultant posts in the emergency department following past recruitment difficulties.
On Thursday, the Department of Health said recruitment for permanent vacancies is led by each individual health trust.
"In the longer term, it is through increased investment in pre-registration education programmes that will create the labour supply necessary to meet the growing demand for services," a spokesperson said.
"The ability to grow our workforce supply depends on the availability of significant, recurrent investment in pre and post-registration training.
"The department and minister will continue to strive to ensure that the department receives the financial resources required to make this essential investment."
'Snowballed'
Dr Fergal Dunn, a consultant in emergency medicine, said smaller hospitals needed to emphasise what they were good at, as well as marketing the surrounding area and lifestyle.
"We set out to actively recruit emergency medical consultants to the Causeway site, it wasn't easy. it was a slow process to begin with, but the interesting thing was once we started to get one or two people over the line it kind of snowballed," he said.
"We went from having one person on the rota to six and actually there are more people interested in coming up here to work.
"There's the golf courses, the beaches, restaurants, we've great schools so we took all that and we're trying to sell the area as much as the hospital and were trying to sell the area as much as the hospital."
The trust's director of medicine, Audrey Harris, said that while there were ongoing issues around recruitment and pay across the health service, it was important to make the post attractive.
"You have to make the post where those people who apply can see they can have a work-life balance, especially medical staff, it is around the job planning, it is looking at special interest, it is looking at career pathways, it is looking at career development."
Dr Fergal Dunne says smaller hospitals need to emphasise what they're good at
A new medical school at Ulster University's Magee campus in Londonderry opened for 70 students last year and will provide additional doctors into the workforce from 2025.
Where to work?
Prof Louise Dubras, foundation dean of the School of Medicine, said the bulk of students would stay within 20 miles of where they trained.
"Where we choose to live and choose to work are influenced by a number of factors but certainly the quality of the working environment and the nature of the support that you get from the leadership in that environment are all really important," she said.
"If we send students to a placement and they have a good experience there and they can see that it's a supportive environment, then they're certainly more likely to want to go back and work," she added.
The Department of Health said no amount of additional funding or workplace planning could resolve the ongoing challenge in recruiting and retaining specialist clinicians.
"It is for this reason the department has commissioned a clinician-led review of general surgery to improve sustainability across the HSC system," said a department spokesperson.
"The department is very aware that the implementation of annual pay awards in Northern Ireland lags behind the other jurisdictions, while every effort is made to implement the awards as soon as possible, the nature of our devolved systems, with annual budgets and approvals locally for pay remits, does impact on the department's ability to respond in a more timely fashion."
In 2018, the department published the 2026 Strategy, a workforce plan for the HSC sector.