Gestational diabetes: Northern Ireland sees 30% rise over four years
- Published

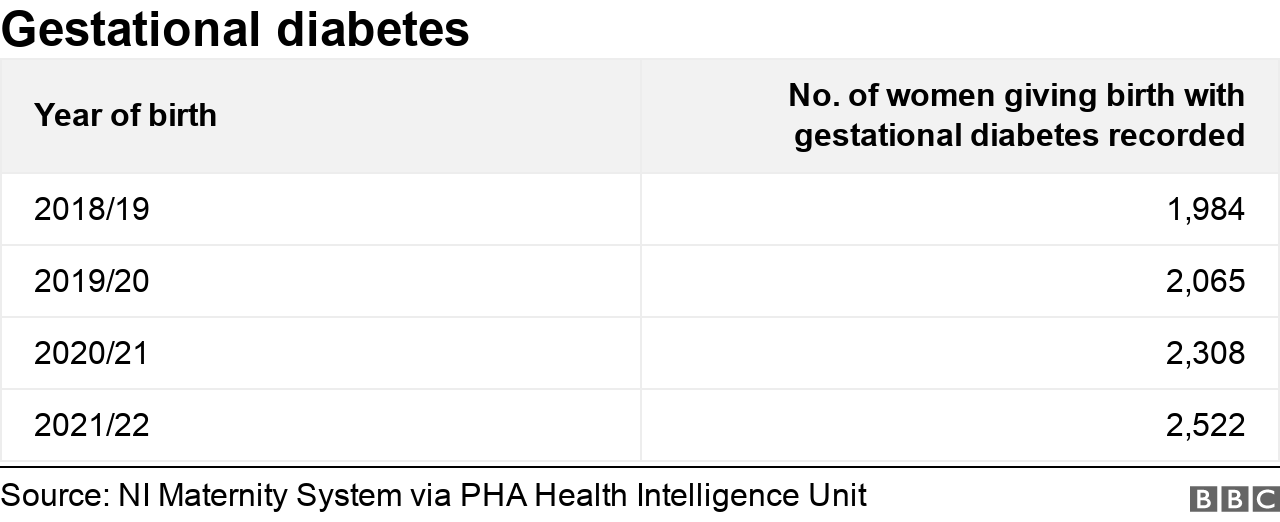
The number of women with gestational diabetes who have given birth in Northern Ireland has risen by almost 30% over the last four years.
Figures from the Public Health Agency (PHA) show more than 2,500 women gave birth with the condition in the year up to March 2022.
Gestational diabetes is high blood sugar (glucose) that develops during pregnancy.
It usually disappears after giving birth.
A diabetes midwife coordinator from Belfast's Royal Jubilee Maternity Hospital said the increase in gestational diabetes could be linked to an increase of type 2 diabetes.
Type 2 is mainly, but not always, lifestyle related and is occurs when the body does not produce enough insulin or the insulin it makes does not work properly.
Gestational diabetes happens when a woman's body cannot produce enough insulin, a hormone that helps control blood sugar levels, to meet her extra needs in pregnancy.
Medical professionals say that while some women may be able to reduce the risk of developing it, the condition cannot be prevented.
It can cause problems for a mother and baby during pregnancy and after birth.

Diabetes midwife coordinator Deborah Burns said there has been an increase worldwide in all types of diabetes
But the risks can be reduced if the condition is detected early and well managed.
In Northern Ireland, the number of women developing gestational diabetes in pregnancy has gone up 27% since 2018.
Diabetes midwife coordinator Deborah Burns said there has been an increase worldwide in all types of diabetes.
"We're not exceptional in Northern Ireland," she said.
"Having a family history of type 2 diabetes will put you at higher risk of developing gestational diabetes," she added.

'It can be very daunting'
Gestational diabetes was a condition Rosaleen Farrell from Rostrevor was aware of, as she has a history of diabetes in her family.
She is now mother to one-year-old Sean and seven-week-old Ellie.
Most women with gestational diabetes have otherwise normal pregnancies with healthy babies but it can cause problems such as a larger-than-usual baby, too much amniotic fluid in the womb, premature birth, pre-eclampsia, the baby developing low blood sugar or jaundice and stillbirth.
Rosaleen was able to control her gestational diabetes in her first pregnancy with diet control but the second time around she was diagnosed earlier and put on insulin as "diet control wasn't going to work for the duration of the pregnancy".

Rosaleen said no matter what you do gestational diabetes "is out of your control" and takes a lot out of you
Rosaleen said no matter what you do gestational diabetes "is out of your control" and takes a lot out of you.
"I'm sure for anybody who isn't aware of gestational diabetes or diabetes in general, it can be very daunting because there are a lot of complications that come with big babies or small babies and pregnancy in itself is difficult without that on top of it," she said.
"You're monitoring your blood sugars all the time, you're monitoring what you're eating, you're monitoring the time you can eat.
"You just can't eat whenever you want to eat.
"It's very hard to be structured like that so that adds an extra anxiety and extra stress during pregnancy."
Rosaleen praised the multi-disciplinary team at Craigavon Hospital for supporting her through her pregnancy.
"Everybody there is doing their bit to get you to the end goal which is a healthy baby and a healthy pregnancy."

Deborah Burns said she can understand why women would be worried when diagnosed with gestational diabetes but they try to screen for it early in pregnancy.
"We give appropriate management, treatment and support and we're aiming for a normal, healthy outcome and a normal delivery," she said.
Ms Burns said women can "maintain a healthy diet and lifestyle before becoming pregnant" as one way to reduce the risk of developing gestational diabetes but it won't take away the risk entirely.
But there are a number of treatments.
These include educating women in making changes to their diet and lifestyle to help bring their blood glucose back into a normal range.
Sometimes medication or insulin is needed.
Gestational diabetes normally goes away after pregnancy but women who have had the condition are at an increased risk of developing type 2 diabetes in the future.
Related topics
- Published20 March 2019
