Dementia patient failed by safeguarding system in Northern Ireland
- Published
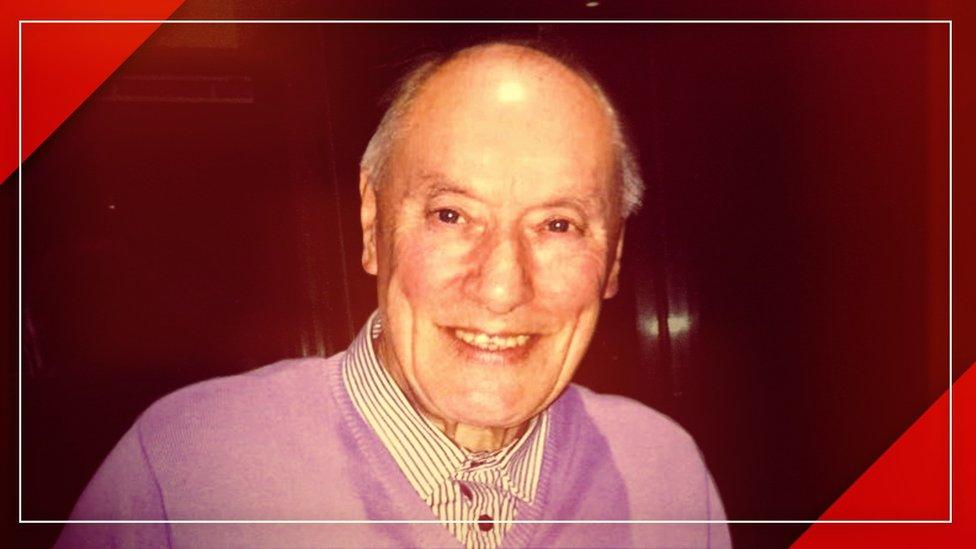
Stanley O'Neill was not showered for three months and was found wrapping a cord around his neck
An elderly dementia patient was failed by the system put in place to protect Northern Ireland's most vulnerable adults.
Stanley O'Neill was not showered for three months and was found wrapping a cord around his neck.
Despite healthcare guidelines, those and other failings were not referred for adult safeguarding investigations.
A review also criticised his nursing home for not being open and transparent with the 79-year-old's family.
Mr O'Neill died in hospital on 20 December 2021.
His family said they had been left "devastated" by a series of failings around his care identified by a Belfast Health Trust investigation.
In a statement Bradley Manor Care Home offered its condolences and apologised to Mr O'Neill's family.
Its spokesperson said: "The safety of our residents is, and always has been, of paramount importance to us but on this occasion we failed to meet some high standards that are rightly expected of us.
"The Covid-19 pandemic was an unprecedented period for the adult social care sector and although we offer no excuses we were faced with unique stresses and an enormously challenging climate."
The adult safeguarding system is meant to protect vulnerable adults in the healthcare system when staff, relatives or patients raise concerns about their well-being.
But in an interview with BBC News NI, Northern Ireland's public healthcare watchdog said vulnerable adults in Northern Ireland were being failed.
'He was our rock'
Sophie O'Neill and her grandfather were incredibly close and she described him as "the rock" of her family.
But when Stanley O'Neill received a dementia diagnosis everything changed.

Sophie described her grandfather as her rock
Things became unmanageable at home and a number of nursing home and hospital stays followed.
In January 2021, during the pandemic, Mr O'Neill became a resident at Bradley Manor in north Belfast. He was placed there by the Belfast Health Trust following a hospital stay.
His granddaughter Sophie said her family began flagging a number of concerning incidents.
She said: "Initially there were two unwitnessed falls at night that we were worried about but then I noticed that his call bell had been removed from his room.
"It was only passed on to us weeks later because I asked staff and they said that he was seen wrapping the cord around his neck and they had removed it."
Sophie added: "I was completely shocked and couldn't understand why it had taken so long to inform his family.
"So for me safeguarding issues were happening and there was no action taken."

Sophie O'Neill and her grandfather were incredibly close
The first time Sophie said she heard the term "safeguarding referral" being used was when her grandfather was taken to hospital in December 2021.
Sophie found Mr O'Neill unresponsive in his room in Bradley Manor and he was admitted to the Mater Hospital in Belfast.
Sophie said: "When I arrived one of the hospital staff said they were concerned about grandad.
"They said his oral care was the worst they had ever seen, and that's when, finally, the hospital started talking about an adult safeguarding referral."
'Failed in care'
Mr O'Neill was admitted to hospital on 6 December and died 14 days later.
His family did not receive a phone call about the adult safeguarding referral until two days after his death and investigators were unaware that he had died.
The case has been referred to the coroner, who will eventually determine the official cause of death.
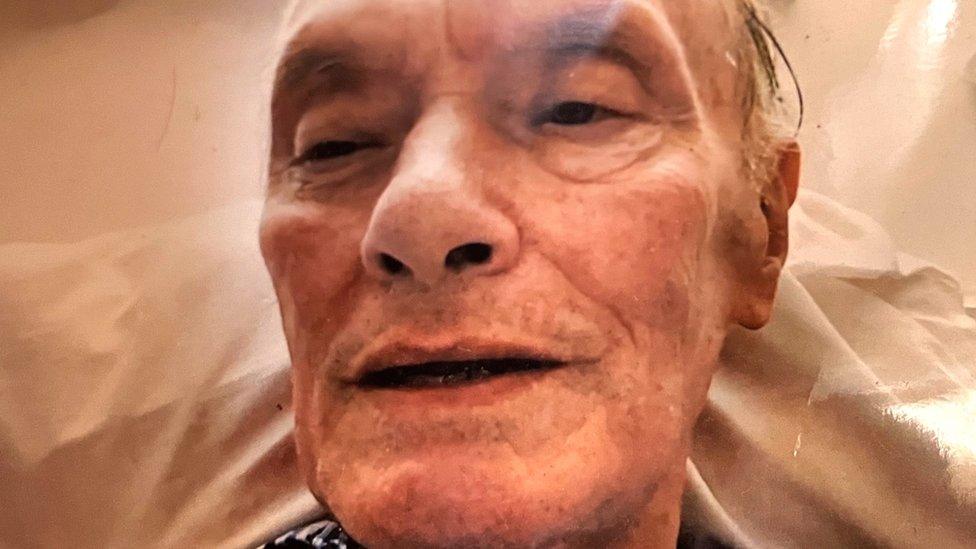
Stanley O'Neill was admitted to the Mater Hospital on 6 December and passed away on 20 December
Sophie said: "The whole point of a safeguarding referral is to protect someone so this was too late for my granddad."
Mr O'Neill's case was eventually investigated by the Belfast Health Trust as a serious adverse incident.
A serious adverse incident is defined as any event or circumstance that led or could have led to serious unintended or unexpected harm to patients.
Investigation reports should be submitted within 12 weeks from the date the incident is reported.
His family received a draft report in April 2023. It found:
in the last three months of his life there were aspects of Mr O'Neill's care in Bradley Manor that fell short of the expected standard
there was a failure to engage with the family to better communicate with them in an open and transparent way
there was a lack of showering during the last three months of Mr O'Neill's life
a failure by the nursing home to provide adequate oral care
incidents of aggression from Mr O'Neill during personal care were recorded by the nursing home
after a number of falls in the nursing home, it did not recommend any changes to prevent or reduce future falls
when Mr O'Neill was found with a call bell cord around his neck there was a failure to respond to it appropriately as an adult safeguarding incident and the family was not informed in a timely manner
staff were not always clear what compounded an incident or how it should be reported
another incident in which Mr O'Neill was recorded as hitting another resident was referred to adult safeguarding. It was considered a symptom of his progressing condition but his family was not informed
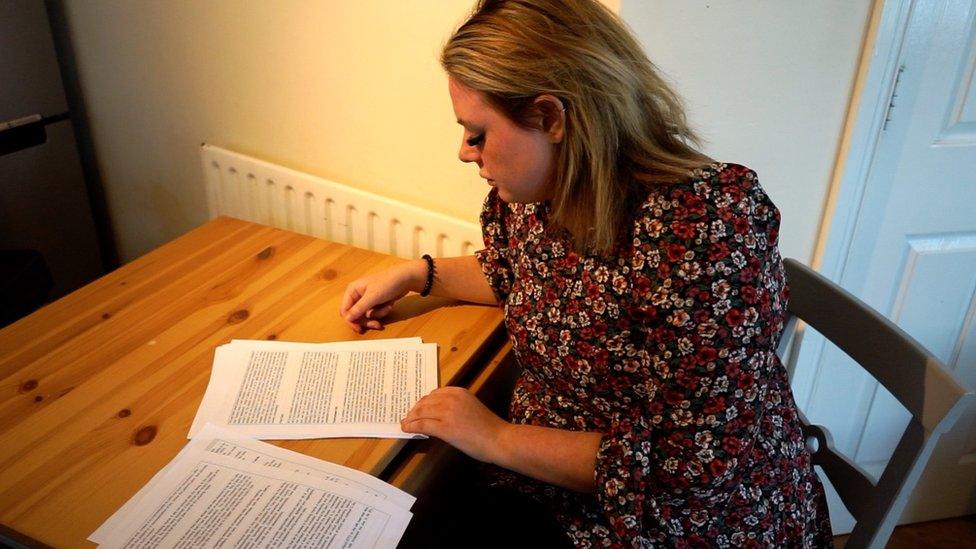
Stanley's family received the draft serious adverse incident report in April
The report concluded that there were failures by all parties involved in Mr O'Neill's care.
Following the report into his case, learning letters have been issued to health and social care staff on how to manage adult safeguarding issues.
'Not fit for purpose'
The number of adult safeguarding referrals in Northern Ireland has increased in recent years from 4,778 in 2019 to 6,897 in 2021.
The Department of Health said the increase could relate to "greater public awareness of adult abuse".
The failings identified in Mr O'Neill's case come as the Northern Ireland Public Services Ombudsman (Nipso) has been raising concerns about Northern Ireland's adult safeguarding system.

"From a number of cases that have come into my office, I think it is clear that our adult safeguarding system is not fit for purpose," said ombudsman Margaret Kelly.
"A lot of the time it is families who have had to draw the attention to healthcare staff about potential failings in care and that just isn't right."
In recent years the ombudsman's office has dealt with eight nursing and care home cases - in seven of those, adult safeguarding was an issue.
The ombudsman cases included:
someone who was wrongly positioned in a bed and, as a result choked, and vomited
a patient who was not appropriately fed and suffered a degree of malnutrition
an adult with a learning disability not given pain relief
a resident who suffered a fractured leg after not being treated appropriately and also choked on her dentures for 24 hours before the care home realised
"Unfortunately while these cases show serious failings, I think they are the tip of the iceberg," Ms Kelly said.

Margaret Kelly is the Northern Ireland Public Services Ombudsman
She added: "Northern Ireland is in danger of falling behind when it comes to protecting our most vulnerable."
Northern Ireland is still the only part of the UK and Ireland without specific adult safeguarding legislation, despite commitments by a number of health ministers to implement it.
The Department of Health said it recognised there were "shortfalls" in the current legislation and a new adult safeguarding bill would be brought forward once the Northern Ireland Executive and Assembly returns.
Bradley Manor said the wellbeing of its residents was its main focus and it had already implemented a number of changes to address the shortfalls identified by the report.
The Belfast Trust said it has undertaken enhanced monitoring at the care home and worked to implement quality and safety improvements.
Reflecting on her grandfather's case, Sophie said: "If any other families go through this I would just advise them to not be afraid to speak up for your loved one."
If you have been affected by any of the issues raised in this story you can visit BBC Action Line.

The Issue: Failed In Care - watch on BBC iPlayer (UK only)
A broken safeguarding system. A family seeking answers. This is Stanley's story.
Related topics
- Published30 November 2022

- Published22 September 2022
