Ethnic minorities' mental health explored at conference
- Published

Beverly Simpson says the idea for the conference came from personal experience
In 2012, during a difficult period with her mental health, Beverly Simpson hadn't slept for two weeks.
She was working as a nurse full-time in Londonderry and caring for her young child.
"I knew at some point I would collapse, but I struggled to ask for help," she said.
Black women are more likely than white women to experience common mental health problems, according to UK government figures, external.
"Culturally, nobody in my community talks about mental health. It's seen as a taboo," Beverly told BBC Radio Foyle's North West Today programme.
She added: "There was no-one who looked like me, that I could relate to or I felt would understand."
Fortunately, Beverly said, her GP did understand and referred her for counselling.
With the right support, Beverly said she was able to navigate her way through her own struggle.
A decade on, that personal experience formed the foundation of an idea to hold a conference to help others.
It led to Beverly, along with the trade union Unison, staging a summit focused on the mental health of black and minority ethnic workers.

Prof Siobhan O'Neill said new communities needed to be able to feel safe
Organisers said the conference, held on Monday at Londonderry's Guildhall, was the first of its kind for Northern Ireland.
Northern Ireland's mental health champion, Prof Siobhan O'Neill, was the keynote speaker.
She told delegates it was an issue she "really wanted to speak publicly about".
"We have new communities coming to us. They need to be able to integrate and feel safe.
"If they are helping us with our health, they need to be well. We've got to get this right and we're not. It's not a level playing field," she said.
Some of those at the conference shared their own experiences with BBC News NI.

Israel Eguaogie said he feared being marginalised because some cultures regard mental health as taboo
Israel Eguaogie said the issue was very close to his heart as a black person who has navigated the mental health system in Northern Ireland.
"Initially the help wasn't there, I struggled to get access," he said.
"Also, in some cultures mental health is a taboo. I couldn't speak to anyone from my own community as I feared being marginalised."
Israel said he would like to see more research and understanding into the mental health needs of black and ethnic minority people in Northern Ireland.
"People can hide behind a lack of cultural awareness and say they didn't simply know. I would like to see training rolled out across the healthcare system."

Lekan Ojo-Okiji Abasi said the lack of diversity among mental health practitioners is also an issue
Lekan Ojo-Okiji Abasi is a clinical coordinator for Counselling All Nations Services- he said that the lack of diversity amongst mental health practitioners was also an issue.
"I attended a conference on mental health, and I was the only black person there.
"More diversity would make a huge difference in terms of overcoming language barriers and understanding people's cultural backgrounds.
"We need resources to train people from minority ethnic backgrounds and encourage them to take up a mental health profession."
Trade union Unison has the largest membership of black and migrant workers in Northern Ireland.
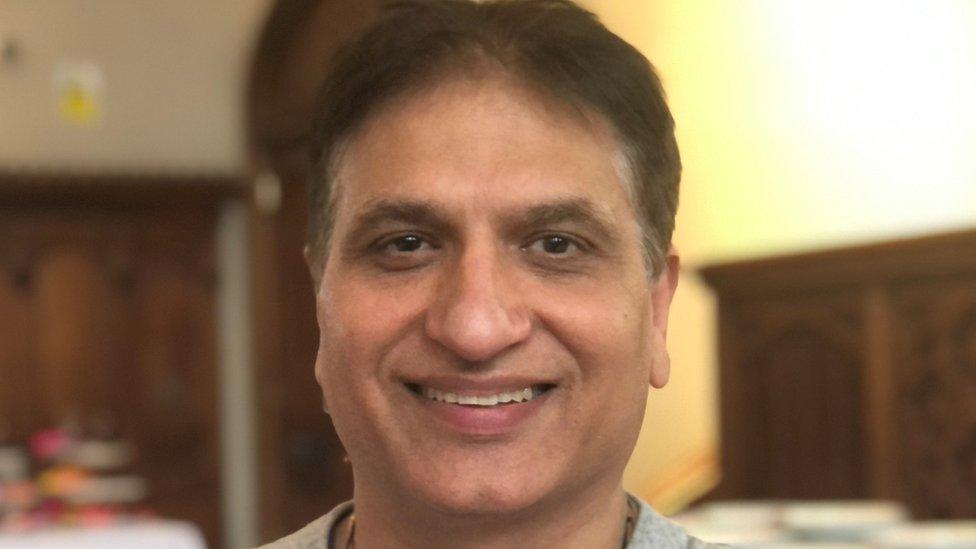
Dr Chugh said services need to take cultural differences into account.
Dr Mukesh Chugh is a consultant anaesthetist at the Western Health and Social Care Trust (WHSCT).
He called for mental health services for minority ethnic people to be specifically tailored.
"People come from different backgrounds," he said.
"I come from India and in some communities there, people are fearful of being open with their mental health condition because of stigma.
"That's why there needs to be more education of practitioners in Northern Ireland.
"People need to be taken with the background knowledge of where they came from. Things can be worked out a very basic level when you take culture into account".
In a statement, the Department of Health said it "recognises and welcomes the increasing number of health workers from a diverse range of backgrounds who are coming to train and work across HSC in Northern Ireland"
It added that the Mental Health Strategy recognised, published in June 2021, recognises a need for a "renewed focus to ensure that mental health promotion meets the needs of those who need early intervention".
"This can include targeted approaches to groups more likely to be adversely affected by mental ill health, including for example BAME groups."
- Published15 February 2023

- Published24 May 2023

- Published7 December 2022
