Community health team 'keeping me alive and at home'
- Published

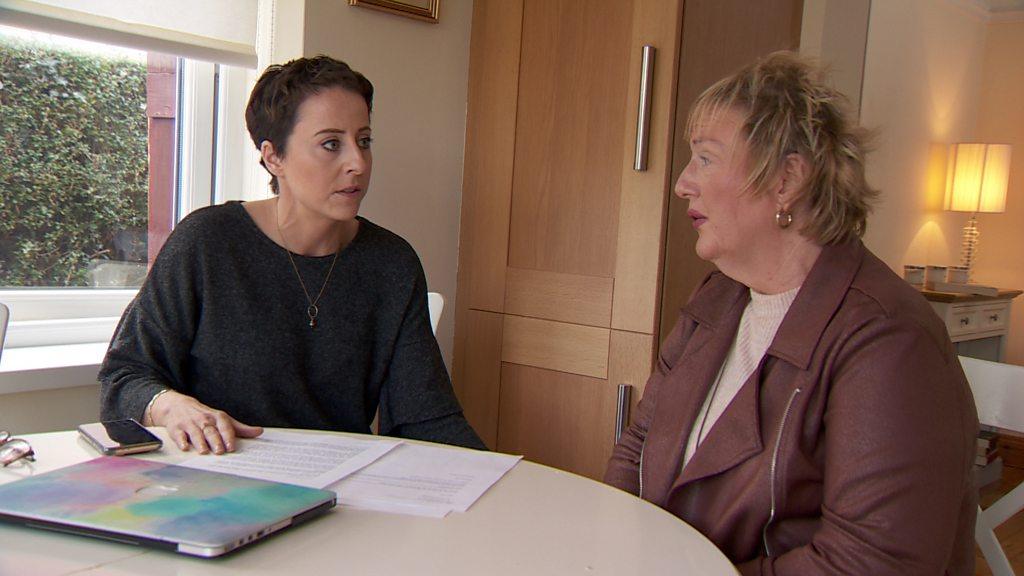
Rosemary Fee said she is treated like a real person by the team
A breast cancer survivor says a community network of health care workers is keeping her alive and out of a nursing home.
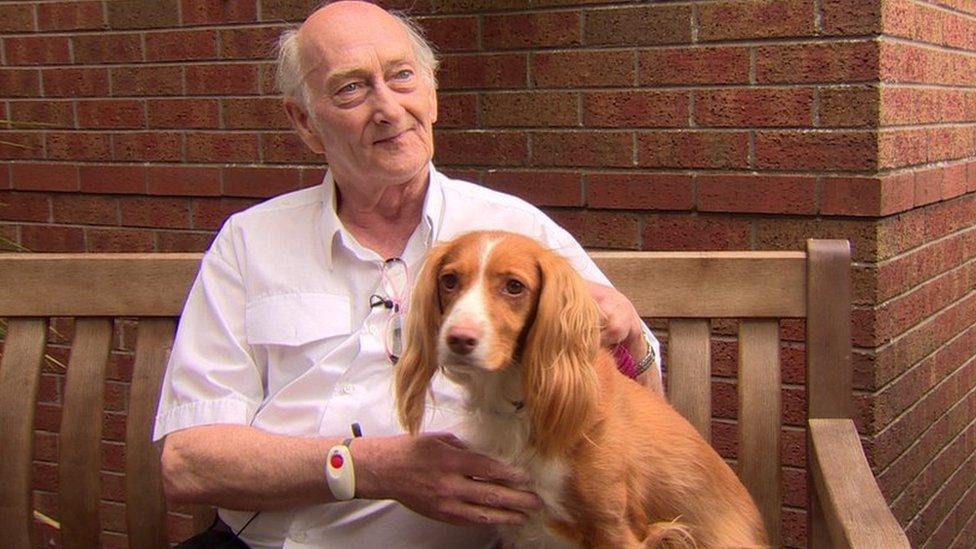
Rosemary Fee lives in supported accommodation in Broughshane, County Antrim.
The 82-year-old said the team treats her like a real person, not like a "wee old bat who can't think for herself".
The care model, run by IMPACTAgewell, bridges the gap between GPs, pharmacists and social workers.
Over the past six years it has helped around 3,000 older men and women to live at home and has reduced hospital admissions.
Speaking to BBC News NI, its executive director for health, Sarah McLaughlin, said they tried to "join the dots between the GP, pharmacist, and the health trust with what the older person requires".
She said in the long run that supported them living independently at home and reduced hospital admissions.
An 82-year-old widow who survived cancer praises her community care support workers.
"We know this model saves money, we know it helps avoid GP appointments and people having to go to A&E," she added.
"We can connect older people back into the community and their surrounding environment, so they feel part of the community.
"We know this model saves lives."
'Get out and about'
Rosemary, who is due her second hip operation in January, said she did not want to spend the last years of her life in a care home.
She currently lives in a two-bedroom apartment with a living kitchen and specially equipped bathroom.
She said she wanted to "live at home for as long as possible" and urged other older people to "get out and about, to go walking and to join clubs".
Having moved to Broughshane in 2020 after her husband died, she said it meant a lot that people know you by your first name.
How does the service work?
IMPACTAgewell has been operating in the Mid and East Antrim area for six years, but the clock is ticking on its funding which is due to run out in 2025.
The hub brings together members of a range of professional disciplines including GPs, community pharmacists and social workers as well as voluntary sector participants to share information and support people.

Sarah McLaughlin said the model helped reduce GP appointments and A&E visits
Social worker Leah Curlett, works for the Northern Health Trust, but is regularly on the phone to the IMPACTAge well team.
"When my team make a referral to Impact, we hope that it will prevent or reduce a crisis occurring in our service user lives," she said.
"They (IMPACT) are able to meet them in their home, assess what is going on and then link them to the right community service which could be about benefits, home safety checks, even befriending them.
"They're the experts, and we rely on their support."
Previous research carried out to evaluate the programme found it resulted in a 91% reduction in emergency unscheduled hospital admissions, along with an 84% reduction in related hospital bed days.
There was also a less substantial reduction in GP appointments and the prescription of medicines.

Pharmacist Ryan McKinstry said he is able to provide face to face consultations
Pharmacists are another vital link in the chain of support.
Ryan McKinstry's pharmacy is based in the heart of a community which he said makes him accessible with "face to face consultations which people want and feel comfortable with".
He added: "We can feed back into the social care team. We are the medicine specialists and can provide that advice."
How is it funded?
The big conundrum for all health providers is getting social care right and keeping older people out of hospital.
There's the added pressure of stretched budgets and getting value for money.
IMPACT which stands for Improving Adult Care Together, is the UK centre for implementing evidence in adult social care.
It is based in the University of Birmingham with the Ulster University in Belfast as its partner.
The national programme is funded by the Economic and Social Research Council (ESRC) and the Health Foundation with the intention that lessons learnt are applied UK-wide.
It has a presence in each of the four nations with IMPACTAgewell operating in Ballymena, Larne and Carrick.
In 2017, it won £1m funding from the Dunhill Medical Trust.
Three years later an external audit found that every £1 spent on IMPACTAgewell generated savings of £2.38 through reduced demand on GPs and hospital admissions.
Those results triggered five years' worth of funding from the Department of Health, but that's due to run out in 2025.

Funding for the service isn't guaranteed beyond 2025
Sarah McLaughlin said they were shocked to learn what they do wasn't already happening in communities.
"When you get to the nub of it GPs don't talk to pharmacists on a day-to-day basis, social workers don't have the time to talk to the community and find out what's happening out there, but being in this position we can bridge the gap," she said.
"Now we need the Department of Health to listen to that and really bring this into the integrated care system."
Back in Broughshane, Rosemary Fee has moved to the community hall where a weekly lunch is in full swing.
A roast dinner, with sponge and custard is served by an army of volunteers.
"Thanks to the team I am nearly back to my normal self," she said.
"The girls come over regularly and are friendly.
"But at the same time, they're asking how you are getting on, they arranged counselling for me and everything to do with my forthcoming hip operation."
Related topics
- Published16 March 2022

- Published23 November 2023

- Published17 May 2023
- Published16 November 2021