NI health: 'My father's care during Covid was negligent'
- Published

Janice Irwin said when she saw her father his hands were stuck together with blood and mucus
A woman whose 84-year-old father died in hospital during the pandemic said she shouldn't have had to "push" for access to see him.
Janice Irwin's father, Ivor Beattie, died in Antrim Area Hospital in April 2021 where he was diagnosed with Covid-19 while being treated for delirium.
Ms Irwin said when she finally saw her father his "hands were stuck together with blood and mucus".
The Northern Health Trust has offered an "unreserved apology".
A complaint made by Ms Irwin against the Northern Health Trust was upheld by the Northern Ireland Public Services Ombudsman (Nipso).
Nipso found "failings in personal care" which would have caused the patient and his family "upset and uncertainty".
What happened?
As she wasn't allowed to visit, Ms Irwin regularly wrote letters to her father so he would know his family was thinking of him.
He contracted Covid-19 while in hospital but Ms Irwin said she was not told.
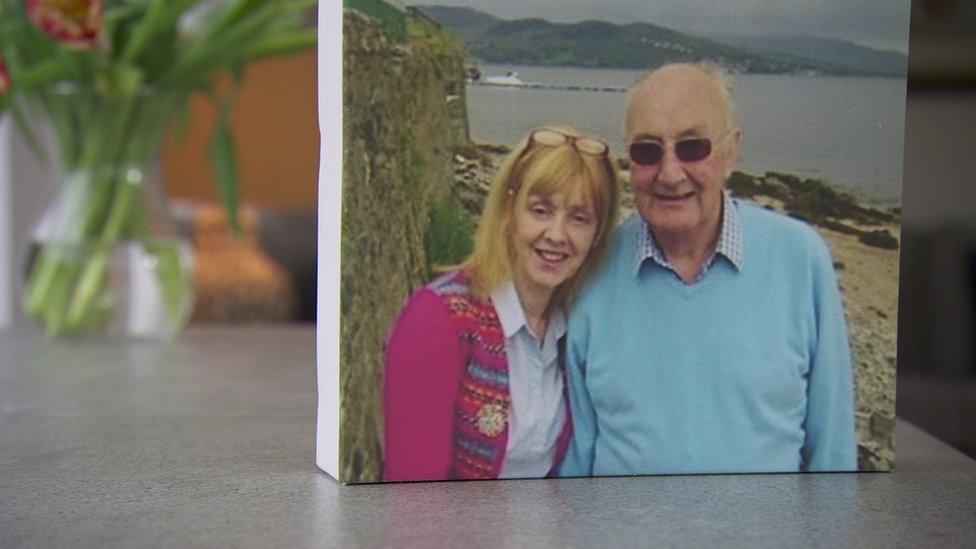
Janice said her she had to push to see her father in hospital before he died
"Mistrust began to creep in," she said.
When she finally "pushed" her way in to see her father, Ms Irwin said she found "his hands stuck together with blood and mucus and his mouth was dry".
"He was so neglected," she added.
Janice Irwin raised several concerns about her father's care including:
the management of discussions about a do-not-resuscitate order
the assessment of his delirium/confusion
the decision not to give him a second Covid vaccination
communication with the family regarding her father's positive Covid test while in hospital
the ability to visit or engage with her father
her father's nursing care especially the development and treatment of a pressure ulcer

Margaret Kelly said the investigation highlights a culture that is defensive rather than open to patients
The Ombudsman, Margaret Kelly, said their investigations highlighted a "culture that is sometimes defensive rather than open with patients, and which doesn't always use complaints as an opportunity to learn and prevent future harm".
Ms Kelly said the northern trust failed to meet the patient's "fundamental physical needs" and as a result it was a "failure in care and treatment - the trust did not have appropriate regard to the patient's rights regarding dignity and autonomy".
Patients 'central to solutions'

The Ombudsman said patients views are central to solutions in improving patient safety
In a statement, the northern trust said: "We have offered our condolences to the patient's family, and we have apologised for the failings subsequently identified in the Nipso investigation.
"We would like to take this opportunity to reiterate this sentiment, and once again we offer an unreserved apology.
"We fully accept the findings and recommendations of the report, and we acknowledge the ongoing distress experienced by the patient's family.
"We are committed to fully implementing Nipso's recommendations, and we will seek to ensure that we continually improve our services, with the report and its findings shared with all relevant staff for learning and reflection."
What did the ombudsman find?
In relation to Ms Irwin's complaint, the ombudsman upheld two and partially upheld one of the seven elements of the complaint.
Two additional failures in care and treatment were also identified.
Among the ombudsman's recommendations was that the northern trust should provide the complainant and family with a written apology.
Another called for the trust to implement an action plan to incorporate a number of recommendations and provide the ombudsman with an update within six months.
The ombudsman also asked the trust to review documentation and practice on the ward in nursing care, particularly in relation to a patient's personal care, monitoring of nutritional intake and mobility.
On Wednesday, a patient safety conference in Belfast heard from experts including Sir Robert Francis KC, who chaired the Mid-Staffordshire NHS Foundation Trust inquiries.
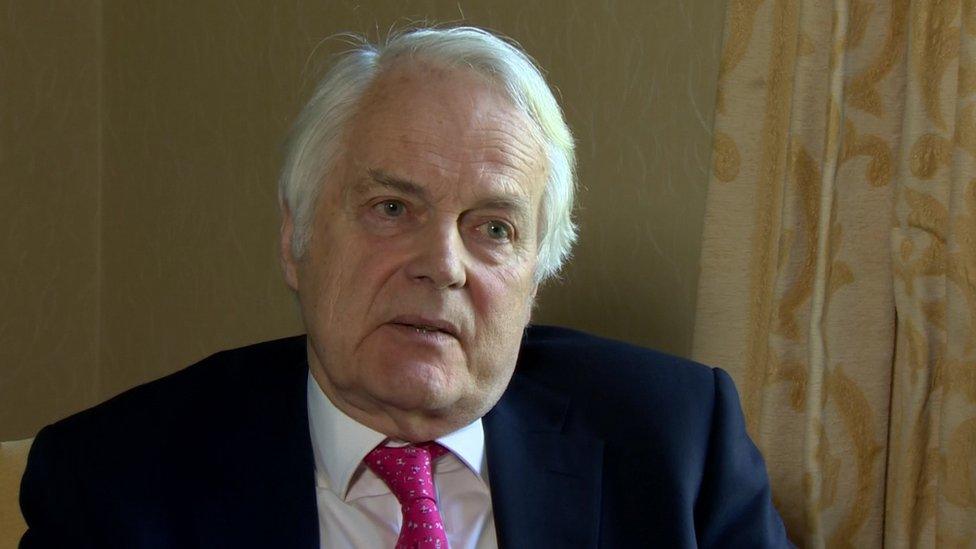
The patient safety conference heard from experts such as Sir Robert Francis
He spoke about the importance of leadership and a duty of candour - ensuring that healthcare providers are transparent with patients and families when things go wrong with care and treatment.
"A duty of candour is absolutely essential for a system of healthcare to be safe," he told BBC News NI.
"It doesn't actually require legislation, although it's good if there is, it will be possible for a health service to implement a duty of candour simply by telling their staff that's what they've got to do."
Janice Irwin also took part, with her story being shared to highlight what can go wrong and how health trusts should deal with complaints.
The ombudsman is expected to call on the Department of Health to take the lead on creating a comprehensive framework for patient safety.