Coronavirus: Worst affected care homes revealed by watchdog
- Published

Care homes have been under immense pressure during the pandemic
A breakdown of the numbers of people who died with Covid-19 for each care home in England has been published for the first time.
Overall, more than 39,000 care home residents died with the virus between 10 April 2020 and 31 March 2021.
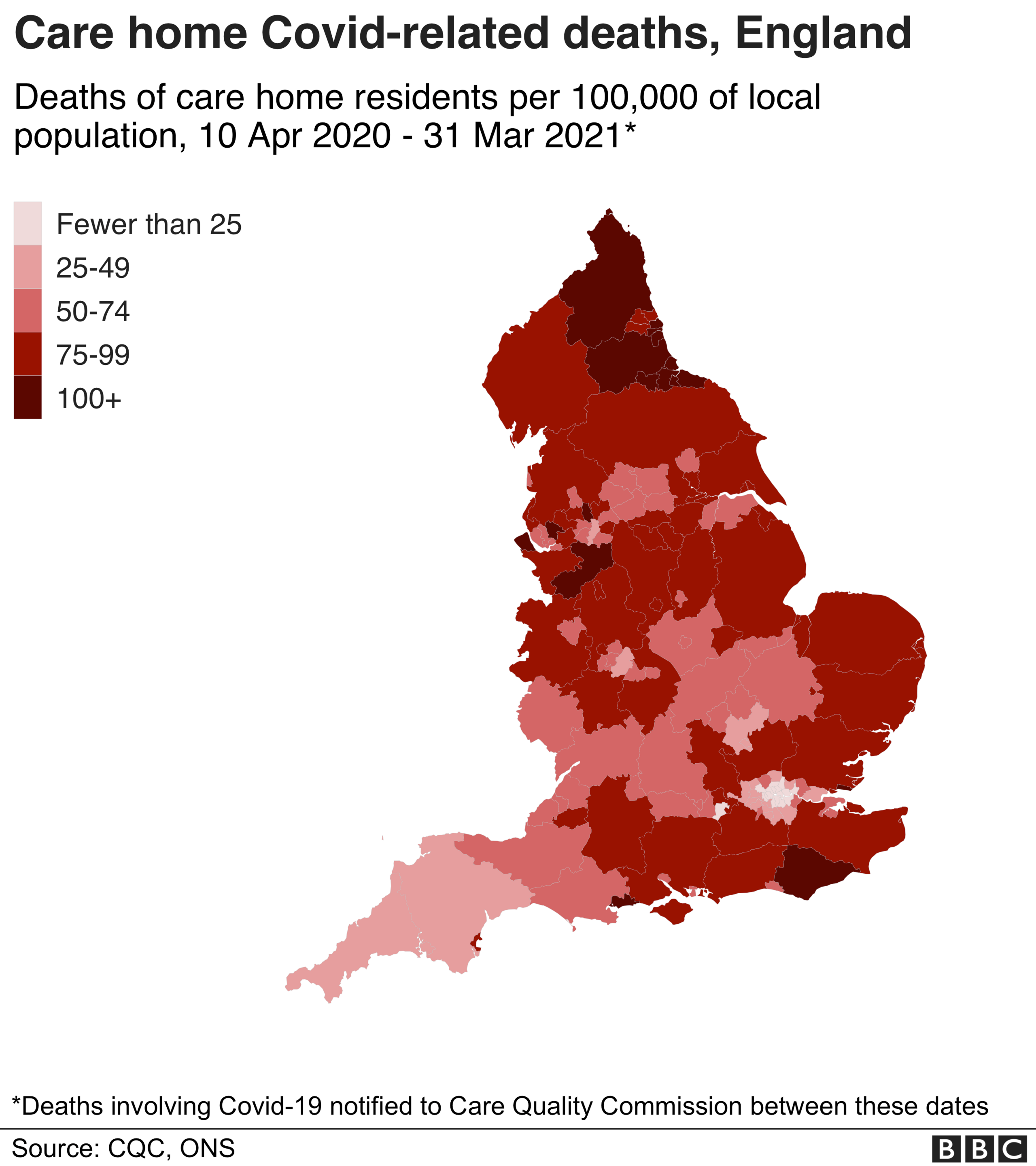
The numbers, released by the Care Quality Commission (CQC), show how the virus spread across the country.
"Every number represents a life lost," said Kate Terroni, CQC chief inspector for adult social care.
The highest number of deaths in a single care home was 44, while 21 homes had more than 30 Covid-related deaths.

Search for a care home

Care homes in the North West had the most Covid-related deaths in the first wave of the pandemic, while those in the South East were hardest hit in the second.
Families who have been campaigning to get the data released say it is vital to have transparency about what happened.
The CQC says it has not found a link between standards of care in a home and the number of deaths.
The regulator adds that many factors are involved, including the levels of Covid in the local community and the age and health of the residents.
Almost half of the deaths - 18,261 - occurred between April and June 2020, with another peak between January and March 2021, the report , externalsays.
Care home managers have a duty to inform the regulator when one of their residents dies.
From 10 April 2020, they also had to say whether Covid was believed to be a factor in the person's death.
The CQC data is based on these notifications.
It also includes the deaths of residents outside care homes, for instance in hospitals.
'They failed my dad'

Amanda Henry with her dad Robert who died with Covid-19 in April 2020
Amanda Henry had been unable to see her father Robert, 78, for nearly four weeks - and when she was at last allowed into his care home in Poplar, east London, it was because he was gravely ill.
Care homes were struggling to get personal protective equipment and the official guidance they needed.
At the time Amanda just wanted to give him some comfort, but even then - in April 2020 - she says she noticed shortcomings with personal protective equipment (PPE).
There was not enough of it, it was flimsy and staff were not using it properly, she claims.
Staff were going from room to room, not changing their PPE, not washing their hands between rooms, and some had no PPE at all, she says.
"What I was witnessing was the virus being spread amongst the residents of the care home in real time...
"I feel it tells us that these vulnerable elderly people were disposable to this government...
"I'm angry, I'm angry that my dad had to suffer like that."
HC-One, which runs the home, says it is deeply saddened by the impact of the virus in its homes and across the country.
In April 2020, it says "we were already working closely with the local public health team to try to keep residents safe and to help them recover, despite the limited information and understanding the country had about this virus at that time.
"Our colleagues were wholly focused on doing the best job they could in exceptionally difficult circumstances, and we are incredibly proud of their bravery and commitment to our residents."
'A living hell'
Sandra Joyce, proprietor of Linden House nursing home in Somerset, managed to keep the virus at bay until December 2020.
"And then it just hit us and just went around the home like wildfire. It was horrific."
By that stage there was plenty of PPE and staff at Linden were well schooled in its use, changing it every time they entered or left a resident's room.
Even so, nearly half of the home's residents died and at one point 80% of the staff were sick or having to isolate.

When the virus hit, it spread like wildfire, says care home proprietor Sandra Joyce
Somerset County Council provided some emergency cover but Sandra still had to stay on until the small hours of the morning, after a full day at work, for days on end.
Staff shortages meant tough choices, she says.
"There comes a point in people's lives when you know there is a point of no return and we always like to have a member of staff sitting with them...
"Instead we had to pop in, pop out."
At one point she decided the home was so unsafe it should close, but was told there was nowhere else for her Covid-positive residents to go.
"So literally, I had no choice."
She fears another wave of the virus would find care homes just as vulnerable.
"It was a living hell, I can't make it sound anything better than that."

The CQC says it conducted 5,577 inspections of adult care providers between 10 April 2020 and 31 March 2021, and that complaints, whistle-blowers and the absence of a registered manager were more likely to indicate poor care than death notifications.
Ms Terroni said the CQC only published the data "once we felt able to do so as accurately and safely as possible", given its complexity and sensitivity.
"As we publish this data, we ask for consideration and respect to be shown to people living in care homes, to families who have been affected and to the staff who have done everything they could, in incredibly difficult circumstances, to look after those in their care".
Care England, which represents independent providers of social care, expressed deepest sympathies to the relatives of all care home residents and staff who have died of Covid-19.
Chief Executive Prof Martin Green said care homes had been "right at the frontline of this dreadful pandemic".
"It would be hugely disrespectful if lessons were not learned at every level," he added.