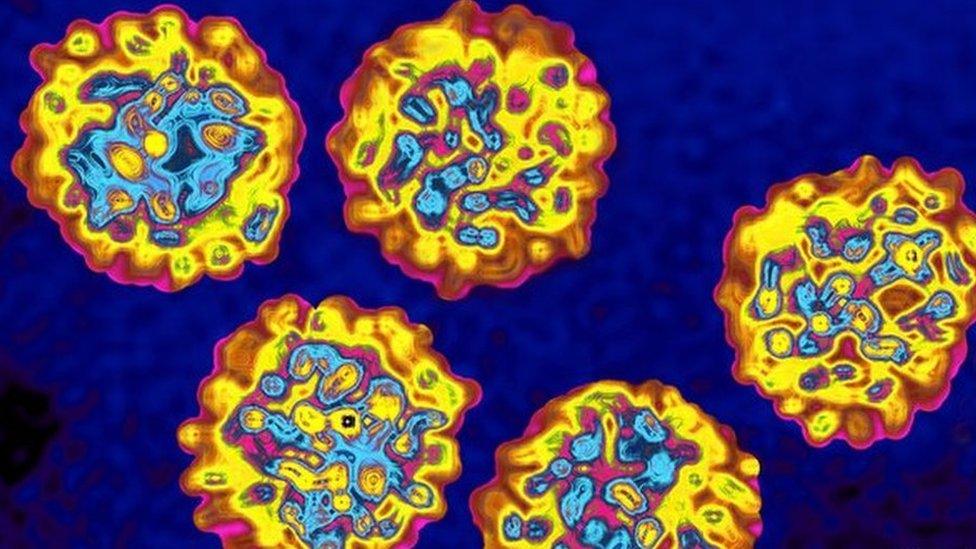
Hepatitis C origins traced back to WWII hospitals
- Published

Conditions in field hospitals meant hepatitis C spread easily between injured soldiers
New research carried out by the University of Glasgow shows that the roots of the hepatitis C virus can be traced back to World War Two and gives a vital insight into how the virus has spread since.
The study, published in the Journal of Virology, dates the beginnings of the hepatitis C virus (HCV) to the 1940s and says it most likely arrived through the mass treatment of soldiers in field hospitals across the country during WWII.
Poor conditions found in these hospitals meant that the blood-borne virus would have spread easily between soldiers as their injuries were treated.
The study links this with the analysis of the number of strains of the virus found across the world, which rapidly increased in the late 1930s and early 1940s, suggesting that HCV was dispersed worldwide during the war.
As the virus was not identified until 1989, infected people returning to their home countries, including Scotland, in the 1940s unknowingly spread HCV through untreated blood products.
HCV infects the liver and causes a chronic infection which can remain undetected for decades due to a lack of symptoms.
The NHS says only around one in three or four patients display symptoms within the first six months, which can include a high temperature, tiredness, and feeling sick.

Anyone who received a blood transfusion before 1991 should be tested for the virus, recommends Lord Penrose
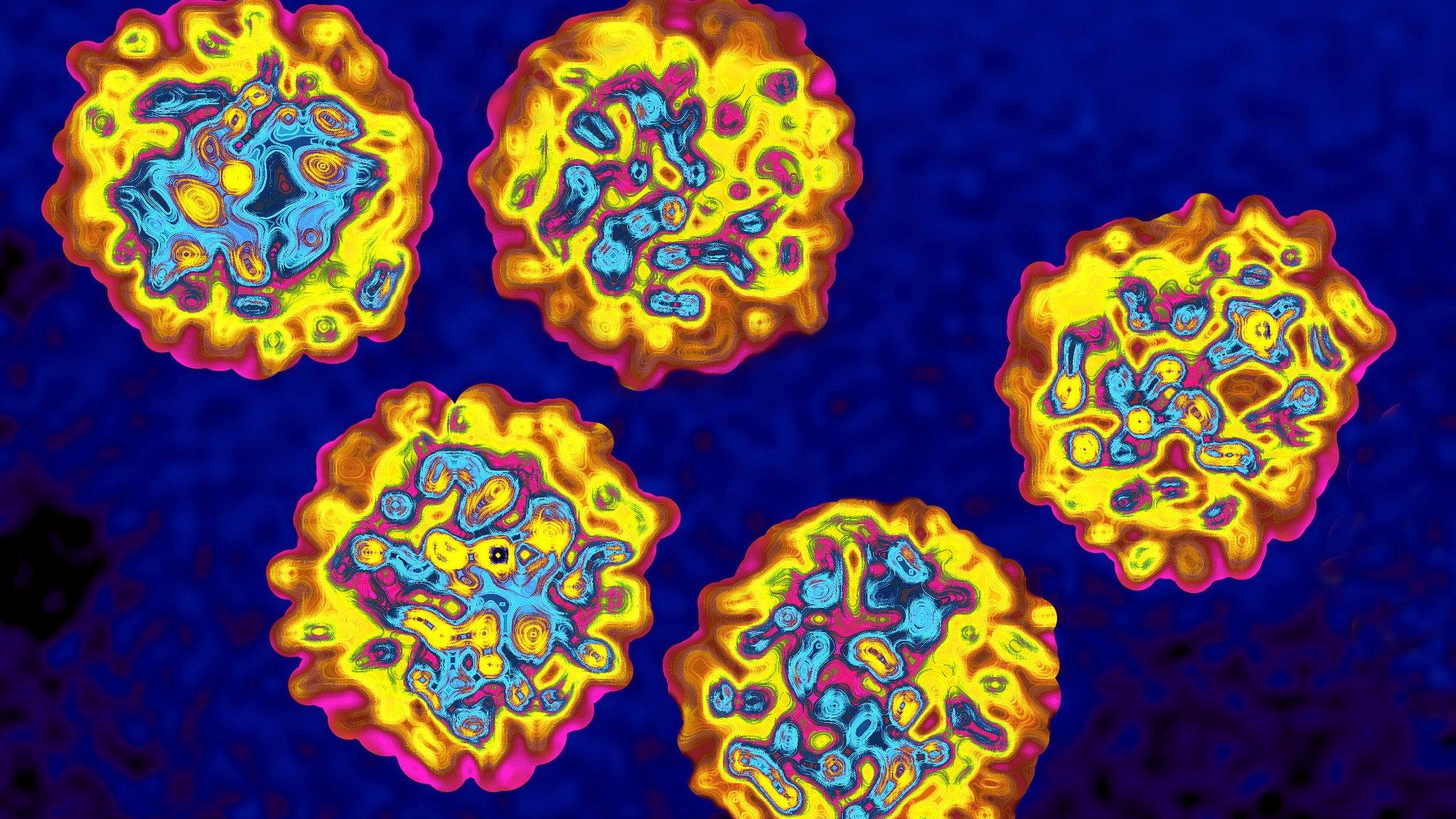
Within Scotland, transmission of the virus began to increase in the 1970s, with different strains being discovered in Glasgow and Edinburgh.
From then until 1991, about 2,500 people were infected with hepatitis C through NHS blood products - mainly those imported from the US - during a contaminated blood scandal described by a Scottish inquiry as "the stuff of nightmares".
Children being treated at Yorkhill Hospital in Glasgow for haemophilia during this time were given plasma products sourced from donors in the US, which were known to be high-risk. As a result, many were infected with HIV and Hepatitis C by the age of five.
Lord Penrose launched a six-year inquiry, the conclusions of which were met with cries of 'whitewash' from angry victims and their families when it was published in March 2015.
The inquiry made one recommendation: that anyone who had received a blood transfusion before 1991 should be tested for the virus.
Dr John McLauchlan, associate director of the Centre for Virus Research, believes the findings of the University of Glasgow's report will help keep spread of the infection at bay in the future.
He said: "Scotland has an international reputation in studying the HCV epidemic that is a global clinical problem, particularly in areas of public health.
"This study gives us a historical record of the spread of the virus in different communities. It will act as a platform for future projects with Health Protection Scotland to follow any strains in the community that may be resistant to these new drugs.
"In doing so, we can support national initiatives that will eradicate HCV infection as a public health concern."
A total 2,500 people were unknowingly infected with HCV between 1970 and 1991 due to NHS blood products
Nowadays, the virus is predominantly associated with the sharing of needles during injected drug use, with an estimated 36,700 people currently infected in Scotland.
Understanding how HCV spreads could support national initiatives such as the Hepatitis C Action Plan to prevent transmission of the virus, to treat people infected and to monitor the appearance of drug-resistant strains.
Lead scientist of the University of Glasgow study, Dr Carol McWilliam Leitch, said: "HCV poses a significant public health challenge in Scotland as well as globally.
"There is currently no vaccine against the virus and the recently developed antiviral drugs are not only extremely costly, but resistant strains have already emerged.
"Pinpointing regions of Scotland driving HCV spread will allow us to more effectively target treatments, monitor their effect and track resistant strains. These measures are essential if we are to combat the virus.
"We now intend to focus our attention on HCV spread in other Scottish regions and to extend the study across the UK.
The study, titled 'Spatiotemporal Reconstruction of the Introduction of Hepatitis C Virus into Scotland and Its Subsequent Regional Transmission', is published in the Journal of Virology and is available in full here., external
- Published12 April 2014
- Published5 November 2014