Doctors prescribe changes to patient care
- Published
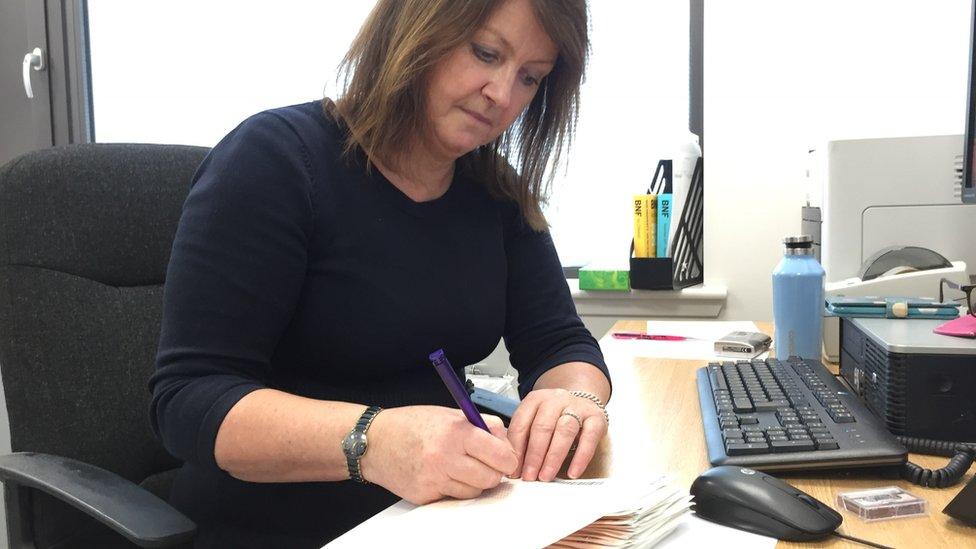
Dr Collette Maule is leading change in GP practice
Scottish GPs have accepted a new contract that will take effect next year but some are already turning their thoughts to new ways of working.
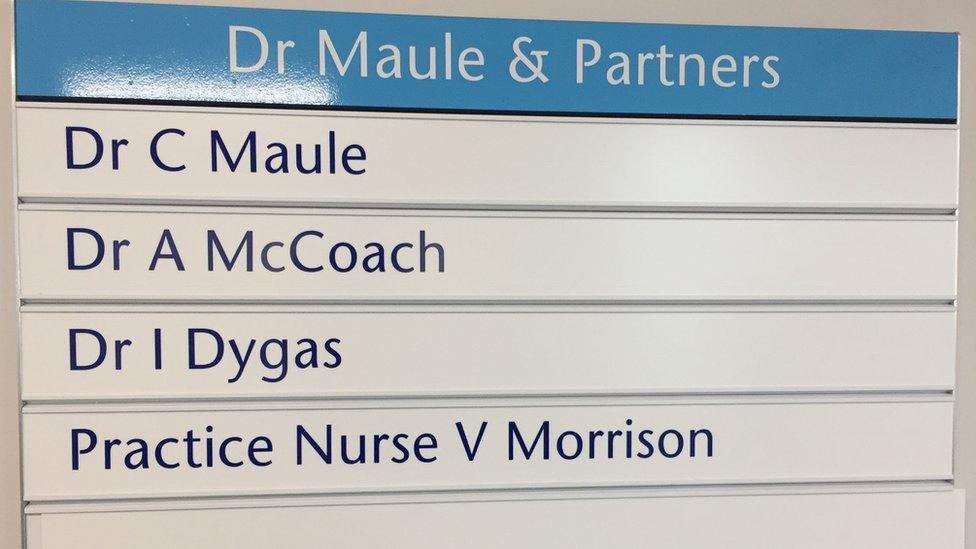
Dr Colette Maule and partners is one of six GP practices based at Wishaw health centre, sharing the building with the local library and a cafe.
Not having to own and run the surgery premises is one of the attractions of this location.
It leaves more time for things medical.
And they kick off when phone lines open at 8am and patients start ringing in for appointments.

Receptionist Kate Girdwood is in the front line, sorting the urgent and the emergencies from the routine or in some cases the unnecessary.
She says: "Every call is different from the last so you never know what you are going to be dealing with.
"It could be a prescription, it could be an appointment, it could be somebody looking to see if they have been referred somewhere."
Delegating duties
Dr Maule was one of the negotiators of the new GP contract, so not surprisingly she is all for it.
One change for her will be becoming even more of a medical leader in the practice in terms of delegating certain duties.
The ultimate aim is to have a paramedic carry out home visits, have specialist mental health and physiotherapy professionals as well as a practice-based pharmacist to sort through and arrange repeat prescriptions.
The idea is that it would free up more time for doctors to spend with patients.
Dr Maule says: "The aim would be, if we had a paramedic attached to the practice, that they would go out and initially triage the patient in the house, if the house call was required.
"They could do blood pressure, listen to chest etc and then phone us back in, the way a district nurse would do, update us on the patient's condition and then we would or we wouldn't need to visit."
Dr Maule says if more time could be freed up then the GPs could extend the current 10-minute appointment slot.
"As patients are becoming more complex, we really should be giving patients more time in the surgery," she says.
"If we can free any time up by using other health professionals then that's got to be everybody's advantage."
Asthma and diabetes
Looking to the future, almost everyone in the practice from the receptionists upwards should have an opportunity to develop more skills and take on more responsibility.
Practice nurse Valerie Morrison already specialises in the treatment of patients with asthma and diabetes.
She says: "There's a lot out here that is totally different to what hospital-based nurses do.
"It's quite a challenging job and a difficult job at times but it is very enjoyable.
"Asthma and diabetes are probably the main specialities where I would probably know a bit more than the GPs and that's where they would refer patients back to me."
Could she take on new skills?
"At the moment I'm not quite sure whether I would want any more," she says.
"I've got enough with everything I do just now, definitely."
Leaving hospital
Some GPs in rural areas remain concerned about the impact of the new contract on their work and in Wishaw one of Dr Maule's GP partners Antonette McCoach says the process of turning round a steady decline in recruitment and retention is likely to take a decade or more.
And with hospitals discharging patients earlier than ever after surgery to free up beds she says it's often GPs who are left to pick up the strain of extra care at home during the post-op recovery period.
"People aren't staying in hospital probably long enough," she says.
"The advent of emergency medicine as a speciality on its own is sometimes seeing people being discharged earlier in the process than they would have been.
"It is maybe more efficient from the hospital point of view but sometimes we are getting people out who are quite unwell and sometimes things aren't followed up on."
Dr McCoach says: "Abnormal results come back two days after they have gone home and then we are left to chase it up."
She says if people require a home visit it is very time-consuming.
"The average home visit can take say 45 minutes and you could be seeing four or five people in that time if they were able to come here," she says.
Patient care
And what of the people this is really all about, the patients who use the service?
How important is it to see "your" doctor versus "a" doctor, or even the practice nurse or another health professional?
One patient, Briony Weir, says: "I like to see my own doctor. I think it just depends on your situation.
"It depends what you are here for. If you are just not well then you can see any doctor."
Another patient, James McCready, says: "You form a relationship with your doctor over time.
"You can speak freely and all the rest.
"If you have to see a different doctor it can be quite embarrassing to start telling your stories over again."
Not seeing patients
During a gap between the morning and afternoon surgeries there is paperwork to be done, and phone calls to be made.
Dr Maule says people don't always understand why not all of a doctors day can be spent seeing patients.
She says: "I'm in the midst of doing patient results, half of which are abnormal so that means I'll have to open up every patient record to have a look at that.
"I've got a whole pile of repeat prescriptions to do. I've got acute results to do and none of that involves me actually speaking to or seeing a patient."
- Published18 January 2018
