NHS at 70: Facing the future with 'never enough beds, doctors or nurses'
- Published

"We will never have enough beds, we will never have enough doctors and we will never have enough nurses," says Steve Turner, a professor of child health and paediatric consultant.
But for him that does not means there is no hope for Scotland's NHS as it reaches 70 next week.
He believes the key to improving healthcare lies in utilising new technologies.
With spending at record levels, people living longer and an ageing workforce how can the NHS stay sustainable for another 70 years?
BBC Scotland spoke to frontline staff about what changes - other than more money - they think could help future-proof the NHS.

The GP - Dr Carey Lunan

The big shift in Scotland's healthcare system in recent years has been away from hospitals and "out" into the community, according to Dr Lunan, chairwoman of the Royal College of General Practitioners.
In the NHS's 70th anniversary year, she says: "There has never been a more important time to think about how important general practice is in delivering a sustainable NHS for the future."
The GP, who works at Craigmillar Medical Group in Edinburgh, says: "About 90% of contacts in the NHS happen out in the community.
"I think to be able to make best use of general practice, and the NHS as a whole, we need to have an open and honest and frank national discussion about how we responsibly and sustainably use our NHS and what we want that to be for in 2018.
"It needs to be a joint discussion which is led by politicians across all the political parties and healthcare professionals, with the public who obviously fund the system through tax."

The specialist - Dr Caroline Whitworth, consultant in kidney medicine

For Dr Caroline Whitworth the focus for the future should be on patient-led care.
What is important for her is "understanding what individual patients want and trying to find a treatment that is most likely to deliver that for them".
"It may not be the newest technology or the newest drug," says the consultant nephrologist, who is based at the renal unit at the Royal Infirmary in Edinburgh.
"Patients are much more aware of their own mortality and they are much more aware of what they want to get out of the life they have.
"Sometimes people don't want to go for the most aggressive treatment, they want to look at something that's going to allow them to stay at home or spend time with their family rather than coming up to the hospital for frequent treatments."

NHS at 70: Facts, figures and challenges

In 2016/17 the NHS in Scotland:
employed almost 140,000 whole-time equivalent staff,
performed 1.5 million hospital procedures,
and conducted an estimated 17 million GP consultations.
So what are the major challenges?
Staffing costs are the biggest expense the NHS faces - £6.5bn in 2016/2017.
The workforce is getting older - 1 in 3 nurses is aged over 50
More money is being spent on drug treatments - £1.68bn in 2016/2017
And in Scotland there are also unique health problems - life expectancy here is still one of the lowest in Europe - 77 for men and 81 for women.

The paediatric consultant - Prof Steve Turner
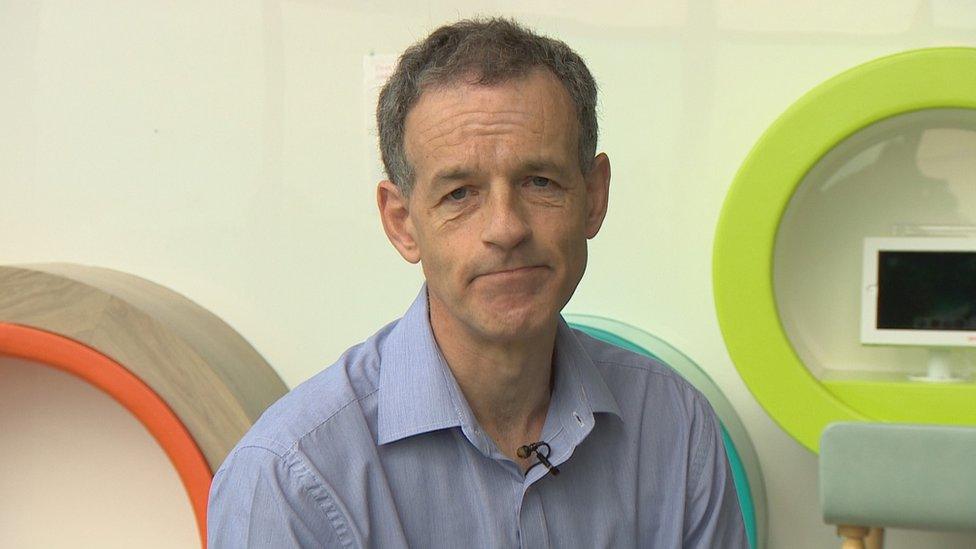
Proper planning and making use of developments in technology and communication will help the NHS improve in the future, says Prof Steve Turner.
"We will never have enough beds, we will never have enough doctors and we will never have enough nurses," he says.
"But what we can do is we can start using the new technologies that are available to us to help improve healthcare."
Prof Turner, who is a paediatric consultant at Aberdeen Children's Hospital, wants to see the NHS make the most of the data already being collected on a daily basis to "help plan the service" for the future.
"We know it is going to get busy at Christmas so what we can do is use that data to predict what the workforce will be required to do and plan the workforce around the service," he explains.
'Shared decision-making'
"A second thing we can do is use communications more wisely.
"For example in Aberdeen we sometimes see patients who have travelled from Orkney or from Shetland or from 60 or 70 miles away. Many of these appointments could be done using video conferencing facilities."
And the professor of child health at the university of Aberdeen thinks "shared decision-making" could also help cut down on unnecessary journeys for patients.
"A child can come to hospital in Huntly, for example, the doctor or the nurse there can see the patient and also bring in a doctor from, Aberdeen maybe, who has got specialist skills.
"The two doctors can make a shared decision in the community and perhaps save the child coming all the way down to the bigger hospital to be seen."

The student nurse - Grant Flannigan

Recruiting more nurses and "getting them young", should be at the core of the NHS's priorities, according to Grant Flannigan.
He is training to be a learning disability nurse at Napier University in Edinburgh.
"I'm really passionate about nursing as a profession," he says.
"I think it's really important for the future of NHS to have more nurses recruited, particularly male nurses.
"One of the best ways to do this is through educating young children, really starting off in primary schools and breaking that barrier that 'nursing is just for females'."

The British Medical Association Scotland - Dr Peter Bennie
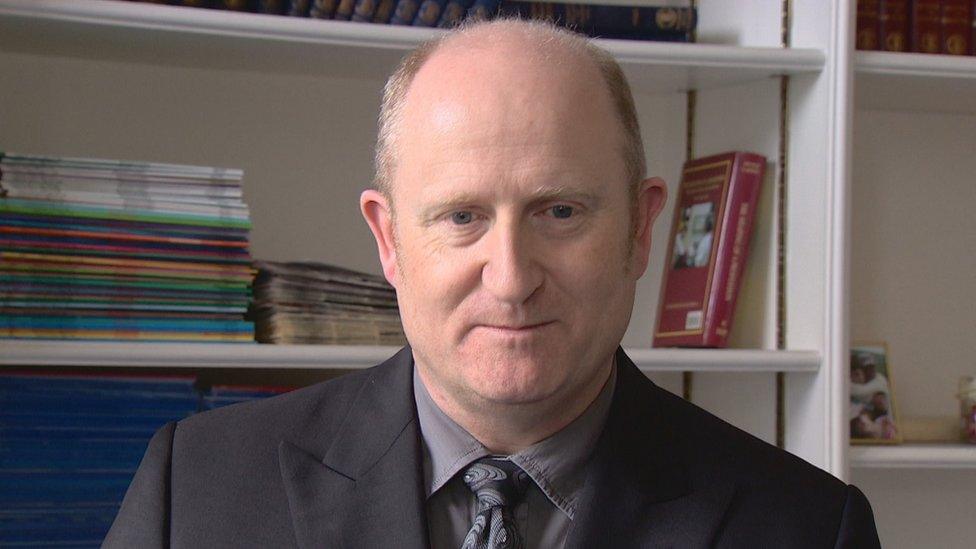
Paisley-based psychiatrist Dr Peter Bennie, who is also the chairman of the BMA in Scotland, wants to see the focus shifted away from constantly trying to meet targets and instead put on measuring "positive outcomes".
And he cannot ignore the need for sufficient funding.
"Even if we get back to, as we should, the 4% increase per year, that at least helps the health service to stand still," he says.
"But even if we get back to that, the challenges ahead are massive and we have to do things differently."
Dr Bennie says: "At present we focus so much of our attention on how the health service works, measuring targets - time to treatment, time in A&E - but not measuring in any meaningful way the actual outcome.
"We need to be looking at positive measurement of patient outcomes rather than time to get to treatment."
- Published17 June 2018
