Maternity and neonatal services to be 'transformed'
- Published

Expectant mothers will be given extra support through a range of new measures designed to transform maternity and neonatal services across Scotland.
The Scottish government is investing £12m in the plan which will also ensure premature babies get specialised care.
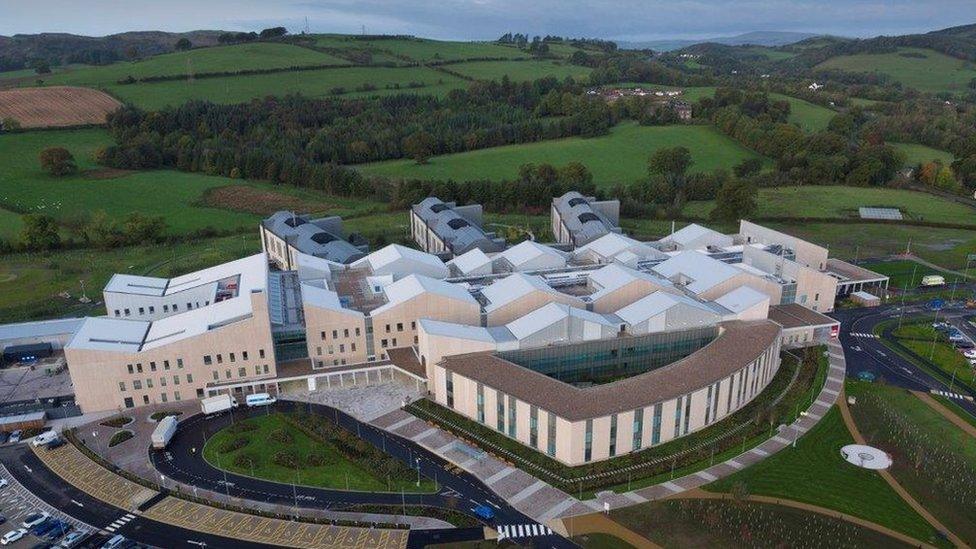
The new model will be tested at four sites, including Crosshouse Hospital in Ayrshire where six babies died "unnecessarily".
Expectant mothers will be cared for by a primary midwife and a small team.
This will continue throughout their pregnancy.
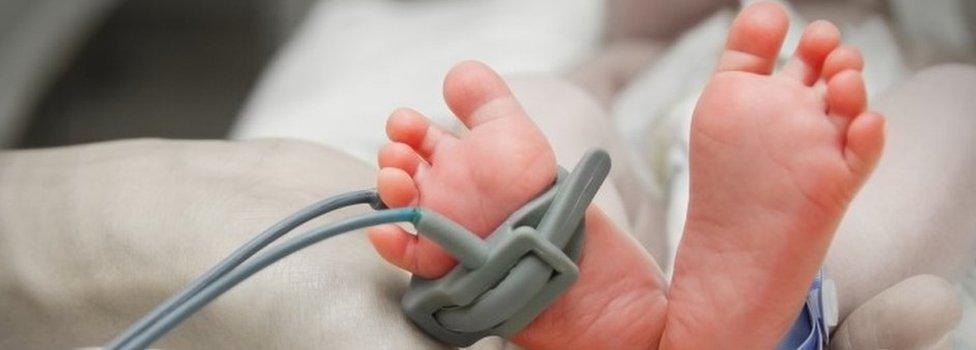
Support will also be on hand to help parents with babies in neonatal units to provide as much day-to-day care for newborns as possible.

New mothers will be given support throughout their pregnancies
The state of neonatal services made media headlines in 2016 following reports of at least six cases of so-called "avoidable deaths" at Crosshouse Hospital in Kilmarnock over an eight year period.
In light of that issue a report was commissioned by the government which highlighted concerns about staff shortages affecting patient care. It also called for improvements in training for maternity staff across the country.
Under the new plan, babies from Crosshouse Hospital who need the most specialist care, will now be treated at the Queen Elizabeth University Hospital in Glasgow before returning to their local neonatal unit.
The new model will also be tested at the Edinburgh Royal Infirmary and Victoria Hospital in Kirkcaldy later this year.

Analysis
By Lisa Summers, BBC Scotland health and social care correspondent
We are two years into a five-year plan to transform maternity services in Scotland.
At the time, The Royal College of Midwives said it would mean a "seismic shift" in care.
Expectant mothers should experience more continuity with a dedicated midwife assigned all the way through pregnancy and birth.
For premature babies, there will be more contact and involvement by parents when in the past they would be kept apart.
However, the sickest and very premature will have to travel further for specialist treatment with the number of intensive care neonatal units in Scotland reducing from eight to three. Experts argue centres of excellence offer the best chances for the 130 or so most vulnerable babies born each year.
One thing is clear, maternity services are becoming more complex with midwives dealing with an increase in older mothers and obesity. It is also against a backdrop where there are midwife shortages. Future planning and investment will be required to make sure such a "seismic shift" has the impact required.

During a visit to Crosshouse Hospital, Health Secretary Jeane Freeman said: "These steps to transform our maternity services will ensure mums, babies and other family members are all supported from pregnancy to birth and after.
"To achieve this, we are looking at community maternity services right through to the care for the most premature babies, where we know outcomes are improved when they are in a unit with a higher throughput of cases and where support services, such as surgery, are nearby.
"We are committed to providing all mums, babies and their families with the highest quality of care according to their needs, backed by this investment of £12m."
Prof Hazel Borland, NHS Ayrshire & Arran nurse director, said: "Our maternity and neonatal teams are dedicated to providing the best possible care to babies and their mums in the safest and most appropriate environment."
She added that the board was striving for continuity of midwife care during pregnancy and "implementing transitional care".
"This change in working aims to keep babies who need a higher level of care and their mums together," she said.
Specialist care
From 55,000 births in Scotland each year, about 6,500 babies need neonatal care
About 4,000 of these are treated in special care baby units and on postnatal wards
A further 1,000 are admitted to a high dependency unit
About 1,500 are admitted to neonatal intensive care
About 110-130 babies are born under 27 weeks gestation in Scotland each year
About 60% of these babies would need to be moved under the proposed changes
The remaining 40% are already being cared for in the proposed three intensive care units
- Published13 February 2019

- Published9 January 2019

- Published6 December 2018
- Published27 June 2017

- Published7 February 2017
