'I was in agony but couldn't get a breast reduction on the NHS'
- Published

Nicole Poole fought for a breast reduction on the NHS for nine years - all while suffering chronic pain in her back
Women have told the BBC they are being refused breast reductions on the NHS despite living with chronic, agonising symptoms for years. The NHS does not record how many patients are turned away but surgeons say more needs to be done.
Nicole Poole pleaded with health service doctors to reduce the size of her breasts for nine years before she finally gave up.
At the age of 18 she began experiencing soreness in her back, which over time led to severe shooting pains down her side. She also suffered migraines which gave her blurred vision, flashes and sickness.
Nicole was convinced it was caused by her chest size - a 32GG despite her clothes being a size 12.

Nicole injured her back while attempting to lose weight for surgery

The condition earned her the nickname "sick note" at work because she had so many absences.
"I was getting migraines twice a week," she said. "I was off work constantly with it. It was a really terrible time. I was depressed, I hated my body and everything about myself. I didn't go out anywhere."
By 21, Nicole's cup size had reached an H and she decided to speak to her GP but was told she was too young for a reduction. She was also advised to consider whether she wanted children before seeking the procedure.
A few years later her GP finally referred her to hospital but she received a letter saying surgery "wasn't necessary".
Nicole, from Cambuslang, South Lanarkshire, said she then attempted to manage her condition with painkillers and developed a serious codeine addiction.
A second referral in her late 20s again led to rejection because her BMI (Body Mass Index) was above the criteria threshold.
Women being 'dismissed'
Dr Judy Evans, honorary secretary at the Royal College of Surgeons in Edinburgh, said far too often women seeking reductions were dismissed because it was seen as a "women's issue" in medicine and that patient's reasons were "cosmetic" rather than practical.
She said: "Breast reduction is an operation which can free people from neck pain, from back pain. It can enable them to do more in terms of good, healthy activities like sport and swimming.
"It can enable them to look after their children better, it takes them off anti-depressants. It's the most wonderful operation in terms of what it does for the person, but also I believe in the long term it saves a lot of money for the NHS."
However Dr Alex Munnoch, an NHS consultant plastic surgeon, said that Scotland had a "very clear" policy on managing breast reductions and that more women were refused surgery because of the "increase in referrals for cosmetic procedures".
He added: "Another concern is that reduction surgery doesn't relieve symptoms. There was a study from a unit in Manchester which showed that for most patients, being fitted with the correct bra could negate a lot of symptoms."
'My breasts were bleeding'
Now 31, Nicole was shocked to hear how other women not only shared her condition but had also been unable to get help via the NHS.
Grace Watt, from Inchinnan, Renfrewshire, was 16 and a size 8 when she started experiencing back pain and migraines - her bra size was a 30GG.
She also experienced painful rashes and said that stretch-marks on her breasts were so irritated, they would often bleed.

Grace frequently had clothing taken in because "nothing fit".

After being told she was "too young" for surgery at 16, Grace tried again after her 18th birthday but despite fitting all the NHS criteria, she was rejected and told she "wasn't a special case".
"I was sobbing," she said. "I was in so much pain and couldn't get anything to fit me. At that point I had a breakdown, my mental health was a mess, I quit my job and on top of the pain I was self conscious.
"I wouldn't show any skin on holiday, I wore T-shirts in the swimming pool and I would hardly go out at home."
'I'll do it myself'
In the past two years, both Grace and Nicole decided to seek reductions through private surgeons - a process that can cost patients about £6,500.
Nicole took out a loan while Grace was helped by her parents but both fear there are more women suffering in silence because they cannot afford to pay for the surgery themselves.

Nicole took out a loan and had surgery privately - she has experienced almost no back pain since

Since her surgery, Nicole has been promoted and works as an opticians manager.
"I was back at work within 10 days and I was fine on paracetamol," she said. "Now I've no back pain and I've had two migraines since getting the operation done.
"I still have anxiety but my depression has lifted. I lost myself for so long I didn't know what I was like."
Despite my pain I couldn't get a breast reduction on the NHS
Grace, an administrator for a charity, said: "When I see pictures of myself I sometimes think 'how did I feel like that?' I was so uncomfortable with myself and I didn't look happy.
"I haven't had migraine since or if I have it's to do with my teeth. I feel more like myself."

Grace said her migraines have drastically decreased

Why are women being turned away?
Many women, including Nicole, have been refused a breast reduction because their BMI was too high. The NHS says it must be 20-27 - the Scottish average in 2018 was 27.7.
NHS Scotland calls this set of criteria their 'exceptional referral protocol, external' which was updated in April this year.
But there has been debate in recent years over whether BMI is the most reliable way to indicate overall health, particularly when bodies are notably disproportionate.
Nicole also pointed out that when she first sought the surgery, her BMI was "healthy", yet she was still rejected.
She also went to great lengths to lose weight on her second attempt but injured her back while exercising.
Dr Evans said: "It's really difficult to have set criteria because this sort of thing should be decided individually, so it shouldn't be based on size or BMI.
"It should be based on the symptoms. And if someone has severe symptoms for any other diagnosis they will get the operations so why should this be any different?"
Are there any other reasons?
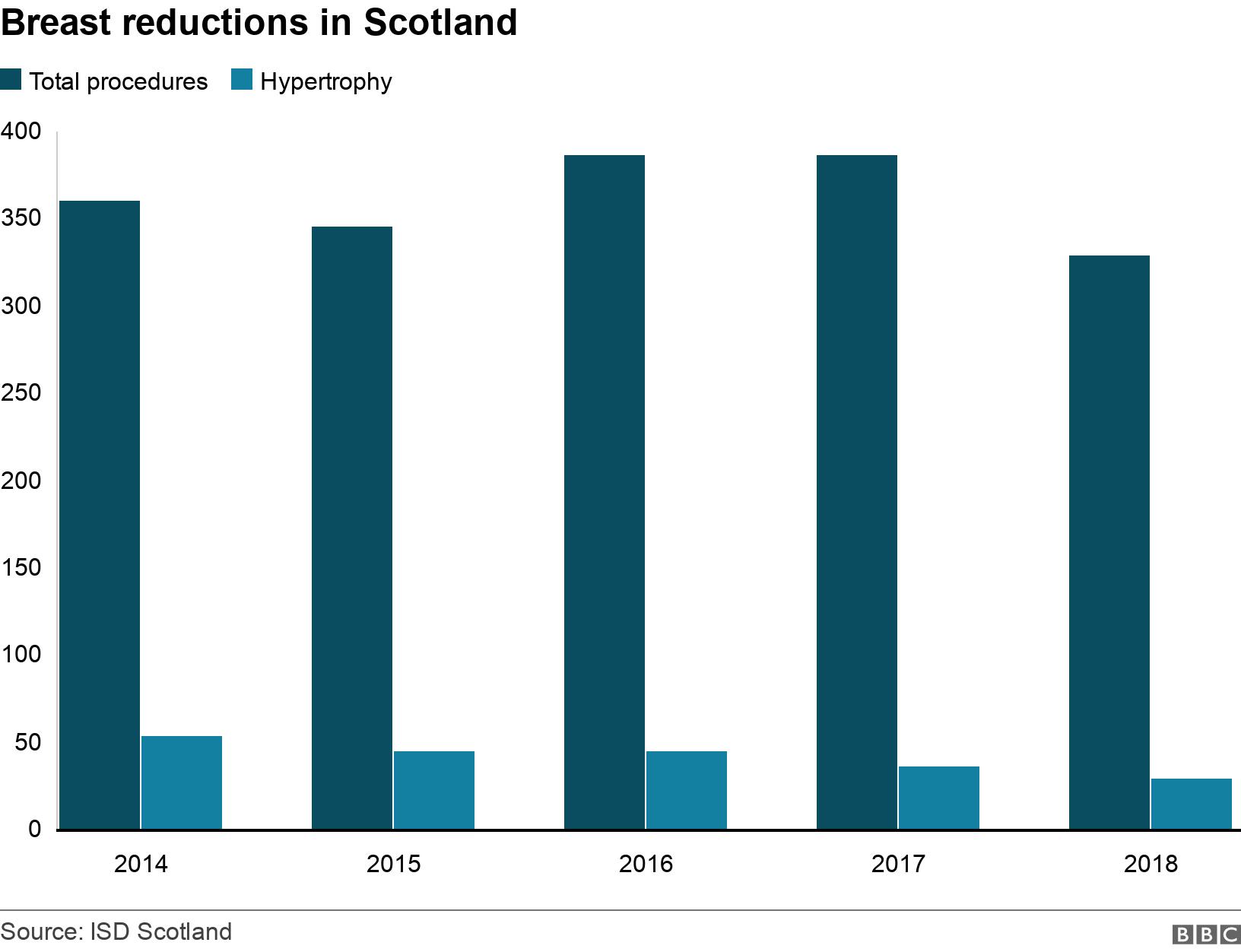
Figures obtained by the BBC show that between 2014 and 2018 the total number of annual reductions was on average 362.
Over a third are women who require the procedure because of cancers, while others receive it to treat conditions like abnormal growths or inflammatory disorders.
The number of surgeries completed for hypertrophy - large cell tissue - was on average 42, and the number decreases each year.
It is impossible to measure the number of rejections because the NHS does not record this figure - only successful surgeries.
The surgeries themselves are costly, particularly for cash-strapped health boards - a reduction in NHS Tayside costs £1,800, for example.
And NHS surgeons say surgical resources are already pushed to their limit and they must prioritise patients who have life-threatening conditions, such as cancer.
NHS plastic surgeon Dr Andy Malyon, who also owns a private practice, said target times "which are set politically" were "enormous".
He said: "What we need to have is some way of defining something that's deliverable.
"The NHS does what it can, I think its [latest] set of criteria is fair and there are a lot of things that should help make clearer that we expect a level playing field across country."
So what can be done?
According to Dr Evans, there should be no debate about the potential benefits breast reductions can give to patients.
She said: "This is something that should not be rationed if it's clinically indicated it can improve the life of the patient, and through them, through all their families."
Having seen BBC Scotland's findings, Labour MSP Monica Lennon, who convenes the cross party group on women's health, said she would ask the Scottish government to address access to breast reduction surgery in its forthcoming women's health plan.
She said: "Private surgery is not an affordable option for the majority of women in this situation.
"Women who experience chronic pain and discomfort related to the size of their breasts need to be taken seriously."
- Published24 September 2019

- Published30 June 2018
