Scotland's hospitals prepare for the Covid-19 peak
- Published

NHS staff must now wear PPE when dealing with Covid-19 or suspected Covid-19 patients
The Western General Hospital in Edinburgh is, in effect, split in two. Red equals Covid patients and green equals non-Covid.
It is remarkable to see what is happening here.
In a place where finding a free bed was usually a rare commodity, wards have literally been emptied.
Operating theatres and recovery rooms are being turned into intensive care facilities in readiness for a rapid rise in cases.
The hospital is already busy treating patients; the first building they reconfigured, usually used for medicine for the elderly, is full.

Wards have been emptied to make space for Covid patients
Site director Chris Stirling, whose job it is to manage this ever changing picture, tells me it is like playing a giant version of computer game Tetris, which can change by the hour.
"The team have done an amazing job over the past couple of weeks creating another 250 beds for Covid response," he says.
"That's involved a huge effort from lots of teams to move a number of wards and departments around while, at the same time, running down some of our planned activity to create the space."
Rapid strategy
I walk through an empty ward. It's eerie. By the end of the weekend they expect it will also be full. Then they will find more.
The Western General has a long history in managing infectious diseases. The hospital was one of the first in Scotland to treat Covid patients.

Dr Claire Mackintosh says it is not something the NHS was expecting to happen
Dr Claire Mackintosh is based here. Her team has been at the forefront of pulling together a rapid strategy to cope with this sudden wave of patients struck down with a virus we know so little about.
She admits she is worried.
"It is not something that the NHS thought, rightly or wrongly, was coming," she says. "We've had lots of really great support from the public but we really need them to stay at home and avoid unnecessary contact with others."

The covid ward was an orthopedic ward a few weeks ago
Dundee's biggest hospital, Ninewells, is also busy and they too must reconfigure at a pace.
Orthopaedic wards, major trauma beds, outpatient departments are all now dedicated to Covid patients.
In normal times the hospital has eight intensive care beds, so far they have created 19 with contingency plans to create 50.
It is clear staff are busy but they are not overwhelmed and those I talk to say they feel safe at work.
The day I visited (Thursday) protective equipment - such as gowns, masks and visors - was only required while in close proximity to patients, who are in single wards as they are assessed.

The higher level PPE is worn for high dependency patients
It was also scaled up to the maximum level for those working in intensive care or high dependency.
But hours later the guidance is updated to say PPE should be worn on all Covid wards.
It is another example of the ever-changing situation in the fight against coronavirus.
I am taken through the wards by respiratory consultant Dr Tom Fardon.
He has been at the forefront of the plans for Covid treatment here in Dundee.
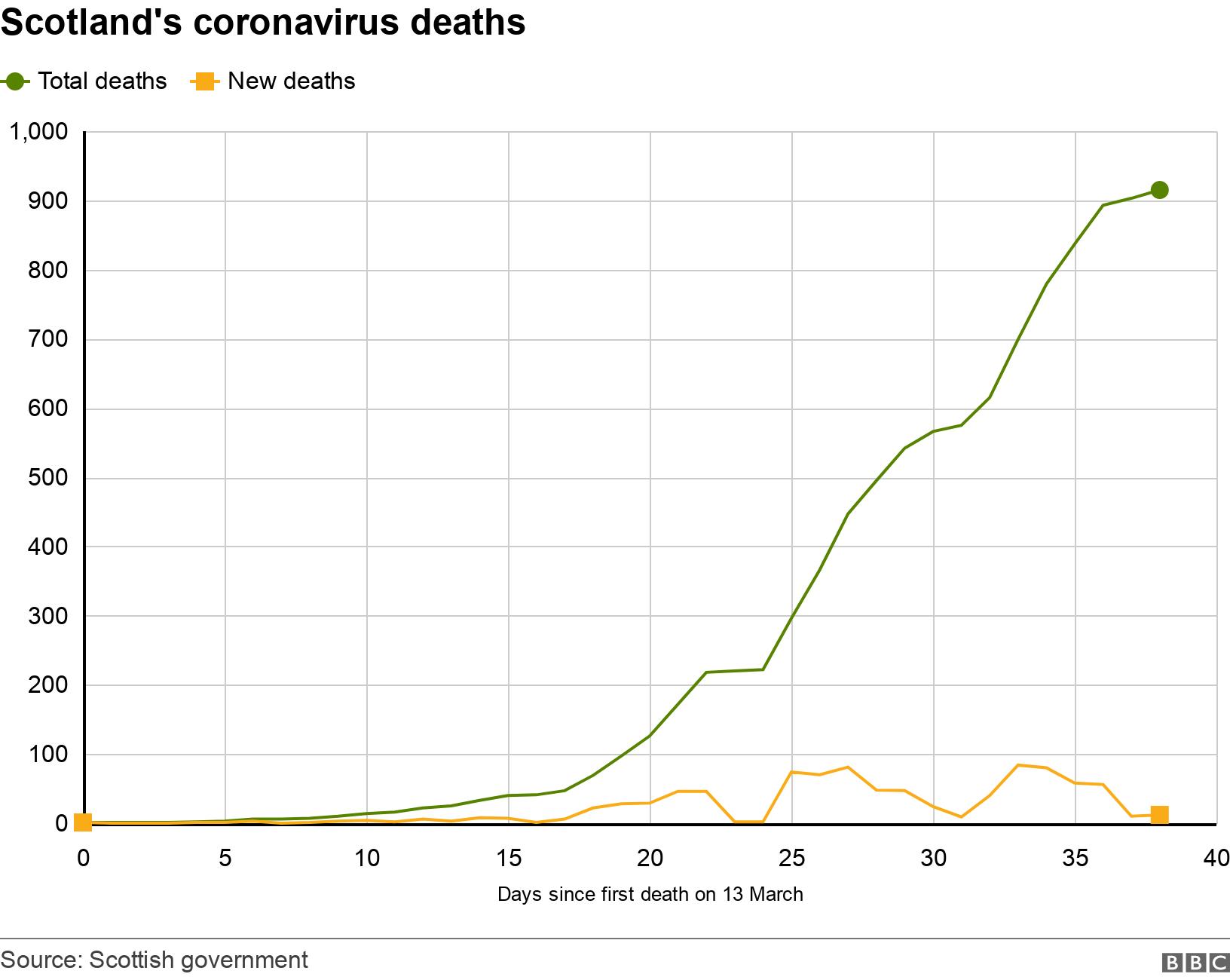
Dr Fardon says the team here do feel prepared. Scotland is a little behind other parts of the UK in the number of cases and deaths it has recorded.
He says he hopes the relatively early introduction of social distancing measures in Scotland will buy them time to stretch out their capacity. But even if they have the beds, they need to staff to be well.
He says: "It's really important that we test staff. Three weeks ago we started an intensive programme of testing members of staff so that we could get them to return to the workforce.

Dr Fardon outside the Covid wards
"As of today over 700 members of staff from NHS Tayside have been able to return to work," he says.
As an observer of the frontline, it is very clear that the NHS is capable of remarkable things.
To even conceive of creating such capacity and so quickly, would have been a distant dream a short while ago.
But staff have rallied together, across health and social care to make it happen.
The future is a worry. In the months to come who will miss out on treatment and what other services will suffer?
But for now, it's all hands on deck to get through the days to come.