BBC correspondent: 'Long Covid has left me exhausted for seven months'
- Published

BBC Scotland correspondent Lucy Adams has been ill since March
More than seven months on from contracting Covid-19, I look fairly normal. There are bags under my eyes but generally I look ok.
It is one of the first things people say: "You look fine - you must be feeling better?" And there is a lesson there.
Over the years as a journalist I have done news stories and documentaries that have touched on the lives of people in chronic pain. The question was how to convey their suffering on camera and get viewers to empathise with something that was essentially invisible?
The answer was to tell the story in their own words. To allow them to give voice to the pain.
I am more comfortable telling other people's stories. But for once I need to tell my own, because I feel I need to explain what "long Covid" is like.
My sick note from the doctor says "post viral fatigue after contracting Covid-19". For me, it is painfully evident but others can't see how it has affected me for months.
How it all began
Like thousands of people around the country I fell ill with Covid symptoms in mid-March.
I am in my early 40s and was generally pretty fit and active, but this hit me hard. My limbs and head ached, my throat burned and my head was foggy. But I managed to lie on the bedroom floor to teach the kids about cheetahs or some such thing.
It was an attempt at home-schooling which often resulted in me falling asleep. I could still walk the kids round the block to get them some fresh air but then I would sleep all afternoon.
After seven days my temperature went up from a fever of 37.7C (100F) to a burning hot 39.4C (103F) and stayed there for 10 days. The pain in my back was agony. My eldest daughter, who was then seven, developed a fever at the same time but she was mainly just tired, while her younger sister had one day of fever and then recovered. My husband had no symptoms.
For me, the illness lingered. I couldn't sleep. I felt nauseous and had horrific abdominal pain. I sweated and shivered all the time. I couldn't stand up but lying down was painful. I was desperate to get a test but, at this early stage in the pandemic, there were none available outside hospitals.
My daughter and I both got a full body rash and lost our sense of taste and smell.
Then came the breathlessness. First from walking up the stairs. Then just lying in bed, it felt impossible to fill my lungs.
I called the NHS telephone helpline and was advised to stay at home unless I couldn't speak at all or my lips turned blue. My daughter became breathless too but then she seemed to recover.
Ashamed of being sick for so long
By the time I had been sick for seven weeks I remember telling my brother I felt ashamed for being off work for so long.
The NHS suggested Covid would last about two weeks yet I was still getting fevers and palpitations and so many other symptoms after two months. It was then that I read a BMJ article by Paul Garner, external, professor of infectious diseases at Liverpool School of Tropical Medicine.
I cried with relief. He was going through the same pick 'n' mix pattern of symptoms. Not only that but he had just started feeling better. He had got ill around the same time as me so I thought that must mean I was days away from recovery.
Unfortunately not.
Prof Garner's next article detailed how he had gone for a long walk and relapsed. He described it as a game of "snakes and ladders" and talked about "phantom speed cameras", external, with which it is impossible to know what the limits are.
Psychological impact of not getting better
On good days I can go for a slow walk - pausing to sit on pavements and fallen trees to catch my breath. I can hold a conversation and pass myself off as fairly normal. On bad days it feels impossible to move from bed. The mattress feels like a ship rolling in a rough sea, my hands shake, my vision blurs, I struggle for breath, my body shivers and vibrates, and every sound cuts through my head like shattered glass.
I've never experienced anything like it. I've had malaria before. Looking back, that was a walk in the park. The psychological impact of not getting better for such a long time is hard to explain. After an illness you would expect a steady improvement and a return to normality. Maybe a couple of days or a week in bed - but it's not happening.
'The time before mummy got sick'

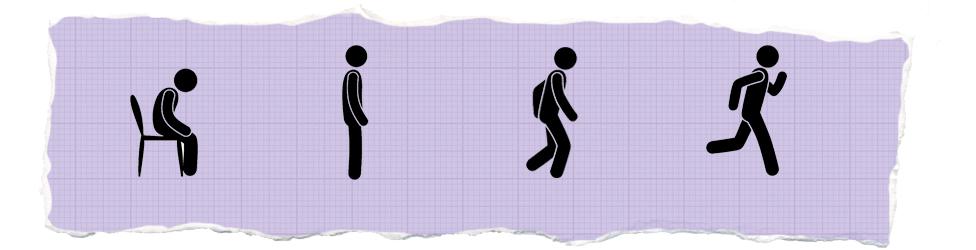
Lucy says she cycled every day before catching Covid now a walk in the park leaves her exhausted
Before I got sick I cycled every day, swam twice a week and went hill-walking when I could. Now a slow totter around the park leaves me breathless and exhausted.
I can still do things but every action has repercussions. If I empty the whole dishwasher at once I might get a migraine so I do one layer at a time. If I go for a walk, I have to go straight to bed afterwards. If I walk too far I might end up with a fever. Vertigo, brain fog, tremors and heart palpitations come and go as they please. And there's the constant sinking fatigue - plus a gnawing anxiety because I don't know when I will get better.
And no-one seems to know what is happening in my body.
My children talk about "the time before mummy got sick" and ask regularly when I will be better. They ask why I can't chase them, can't play ball. Why I can't get out of bed to walk them up to school.
I drop pans when cooking for them as my hands shake so much. The other day I keeled over in front of them because of vertigo. My eight-year-old daughter still has some symptoms. She is back at school but is easily fatigued and has heart palpitations. She can climb trees but walking up stairs leaves her exhausted.
We have both had extensive blood tests, chest x-rays and heart scans. We've both been told to wait and rest and pace but for how long? And how can I explain pacing to an eight-year-old if I can't get it right myself?

LONG COVID: What is known about it?
FACE MASKS: When do I need to wear one?
LOOK-UP TOOL: How many cases in your area?
What is long Covid?
Data analysis by Kings College London suggests about one in 20 of those people who contracted Covid-19 in the UK are suffering long-term symptoms. One in 10 are suffering for three weeks or more.
Tim Spector, professor of genetic epidemiology at King's College and leader of the Covid Symptom Study app, says about 300,000 people in the UK have reported symptoms lasting for more than a month - so called long Covid. Data from the app shows about 60,000 people have been ill for more than three months. He says the more we know about Covid "the weirder it gets".
There are growing concerns about the impact of post-viral inflammation and long-term damage to organs and the cardiovascular system.
On Facebook and Slack thousands of people in the UK and abroad have joined long Covid support groups where mothers and fathers, sons and daughters describe an enduring medley of symptoms including shortness of breath, fevers, heart palpitations, gastrointestinal problems, headaches, sore throats and chronic fatigue. Many of those on the groups were formerly healthy and active and don't fit the demographic of those we were told would face the greatest danger from the virus.
Many are in their 30s, 40s and 50s. There are marathon runners, cyclists and gym-goers, parents talking about young children with long Covid, and students in their 20s. Most are struggling to get support. Some tested positive for Covid-19. Others, like me, fell ill when there was no testing available.
For those of us on the Facebook Long Covid Support group, this is one of the only places to get help.
When my hair started falling out by the fistful in the summer, other members explained the same was happening to them.
Prof Garner tells me that currently he feels "many of the patients know more than the doctors". He says it's time to start sharing that knowledge and ensure there is proper medical screening of those with long Covid.
No-one can explain how long it will last
My GP has been vigilant. Consultants have been interested and ruled out everything other than Covid-19 but no-one seems able to explain how long the symptoms will last or how to get rid of them.
One consultant explained that even though the live coronavirus has effectively died, my body still thinks it is there. It has become a ghost in my system and every day I exhaust myself fighting something which isn't there. A cardiologist explained to me that the virus can knock out of kilter the normally automatic systems - heart rate, breathing, body temperature. All things which seem pretty important.
Some doctors, patients and academics are campaigning for more research and rehabilitation for long Covid sufferers. The UK government and NHS England have said they are working on Covid rehab centres and community services for every part of England.
But as it stands many areas don't have such centres, and people on the long Covid Facebook group are struggling for medical and psychological support. Many feel they are not being listened to.
The Scottish government has talked about a long Covid "framework" and person-centred rehab. But when I ask my GP for a referral to a rehab centre she says they've been told nothing about their existence. The NHS says it now officially recognises long Covid but even the doctors I've spoken to feel they are struggling to access tests, care and support. For most it's a question of being left to fend for yourself.
I'm lucky though. I've got a supportive husband and family, enthusiastic young children who make me laugh and great friends who keep in touch. And I've still got a job to go back to.
Many others have not been so fortunate. I've spoken to people in Scotland and elsewhere who have lost their jobs because they were off sick with long Covid. Others, including cleaners and care staff, feel they've been forced to go back despite all the symptoms because they're on zero hours contracts or have run out of sick pay.
It leaves serious questions for employers and government at all levels on how to support those suffering long Covid.
No end in sight
I assumed I could push through this illness. That I could drive my way out of it through exercise and good diet and supplements. It has always worked in the past. It turns out that is not the case. And some small-scale recent studies suggest that trying to push through could actually make things worse.
In January our then seven-year-old daughter was so anxious about coronavirus coming to Scotland that we showed her how far away China was on the map. We said that even if it did reach here it would only be like getting a bad cold. It was a grossly inaccurate forecast.
About 1.25 million people have died worldwide. Families have been devastated.
Everyone is coming to terms with a new reality.
As the number of people struggling with long Covid increases, it feels important to shift the narrative away from just focusing on how deadly the virus can be. There are thousands of people with long-term effects who still don't have an end in sight.
- Published24 October 2020

- Published15 October 2020

- Published6 October 2020

- Published3 July 2020

- Published23 May 2020
