Covid in Scotland: An intensive care night shift 10 months on
- Published

At 5am, staff nurse Natasha Cumming tends to the ventilation tubing of a Covid-19 patient
In April, at the peak of the first wave of the Covid pandemic, I was given exclusive access to the intensive care unit at University Hospital Hairmyres in East Kilbride.
Those images were among the first in Scotland to show an ICU treating people infected with coronavirus.
Ten months later, I returned to capture another Hairmyres ICU nightshift, as it deals with a further wave of seriously ill patients.

Dr. Austin Rattray leads the ICU nightshift.
He says: "There is an element of fatigue, but we anticipated that we would be back here again, especially in the ICU, and now the third peak is here."

Dr Maria Smith leads a team of five to prone a patient. The delicate process of turning ventilated patients has become routine for the staff, and is still a primary treatment for critically-ill Covid patients.
Last year, these doctors and nurses were still learning how to treat what was then a new virus.
Now their methods have been adapted, studied and standardised.
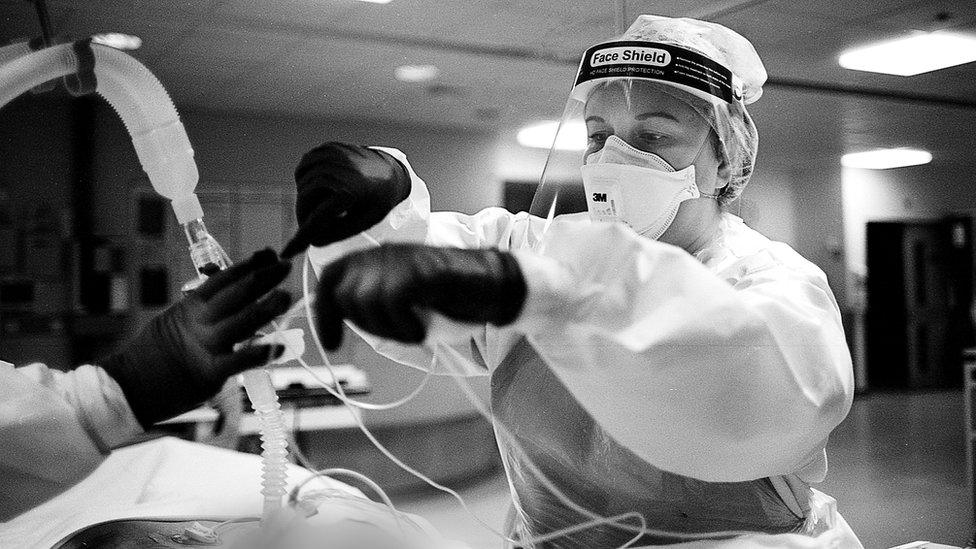
ICU charge nurse Morag Malcolm helps arrange the delicate web of monitor wires and the ventilation tubing that keeps a Covid patient alive.
"We're all fatigued emotionally and physically, but we look out for each other," she says. "I do wonder if when things calm down if it will hit the staff harder, when we have time to reflect on the loss we've seen."

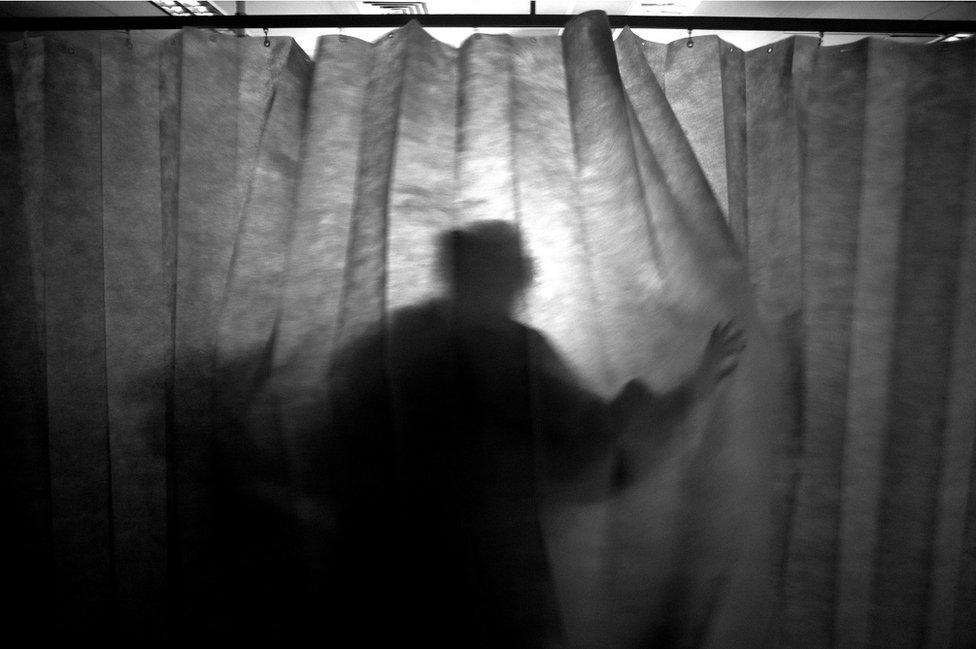
Without families allowed in to visit patients, nursing staff have become both a proxy for, and bridge to, family outside the hospital.
Nurse Natasha Cumming says: "We get to know the patient but with Covid we're not getting to know the family, which personally I find difficult."

A Covid patient in the ICU is likely to be intubated and put into an induced coma.
The patient here doesn't know that a nurse is keeping them fed, lifting them to keep air in their lungs, or holding their hand through the night.
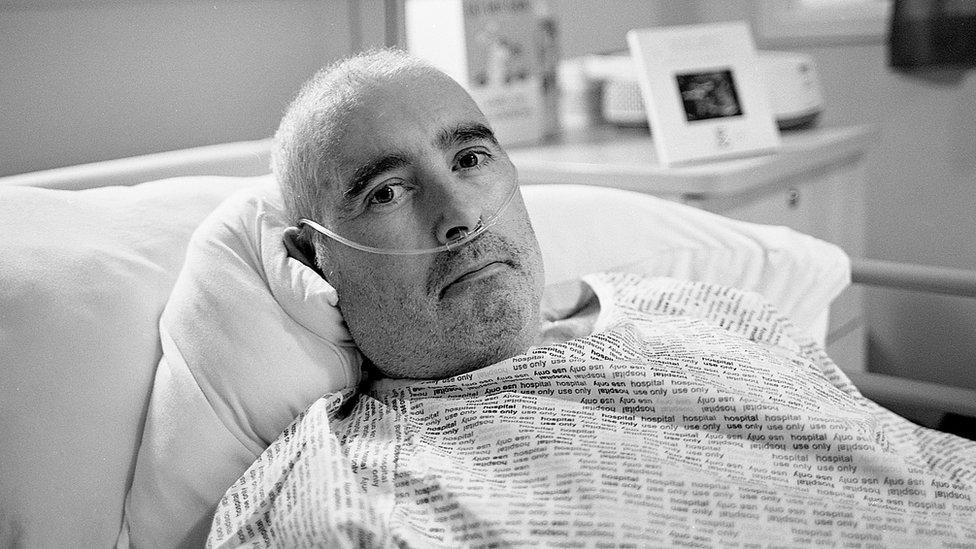
Brian Fernie is recovering after 67 days in the ICU - 61 of them on a ventilator - longer than any Covid patient in the Hairmyres ICU.
The window fitter from Cambuslang awoke to find his muscles had atrophied and he must relearn how to walk. But good news was also waiting, his daughter had been pregnant before he was put under and was finally able to tell him he was going to be a grandfather.
Despite new treatments, 30% of Covid patients who required ventilators in this ICU have not survived.

The team is still made up from both ICU specialists and other hospital staff with transferable skills, who have been drafted in.
"There's no question about it, staffing is our biggest problem now," says Dr Rattray. "The treatments and logistics have improved, but you can't upscale ICU staff that quickly, it takes years to train an experienced ICU team."

Dr Marielle Li has been transferred to the ICU from her primary, pre-pandemic work, in operating theatres.
"Everyone's life has been disrupted by Covid," she says. "But part of the fatigue we feel is that we're not getting to our normal workload, but those problems haven't gone away."
While Covid treatment is prioritised, a backlog of other patients keeps building and staff anticipate yet another wave of intensive work from those treatments.

Dr Rattray and team gently lift a patient's head to improve his breathing.
He says: "We had a dip in morale after the first wave, that happens after a traumatic experience. But the team is resilient and we've pulled together to provide compassionate care, and we'll keep doing that."
All pictures by Christopher Bobyn
Related topics
- Published1 May 2020
