HRT drug to be reconsidered for use in Scotland
- Published

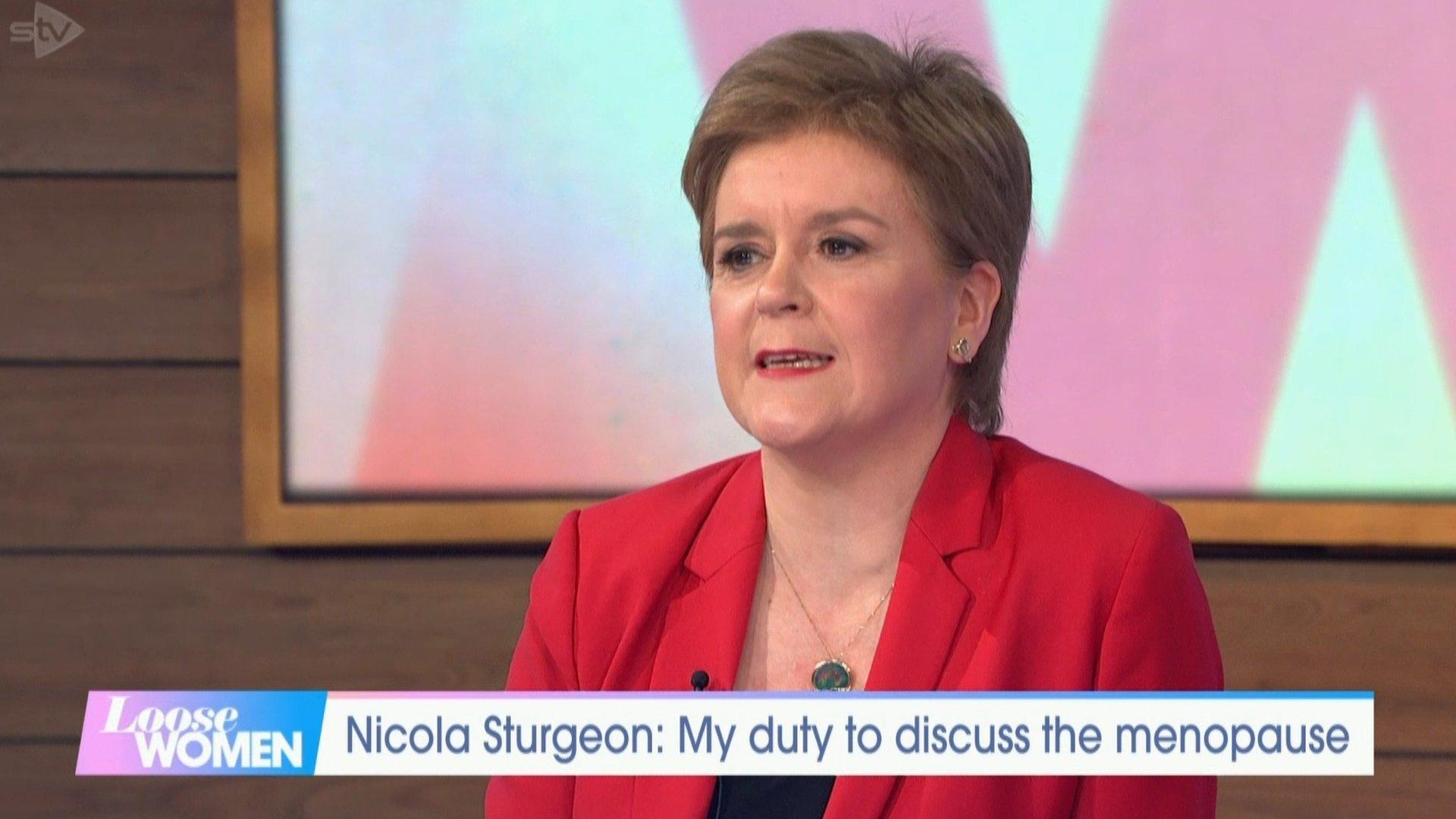
Davina McCall has become the face of menopause health for many women in the UK after her documentaries on the previously taboo subject
A sought-after hormone replacement therapy for women in menopause is to be reconsidered for use in Scotland.
The Scottish government said it had encouraged the maker of Utrogestan to resubmit its medicine to the Scottish Medicines Consortium for approval.
Earlier this week, TV presenter Davina McCall highlighted that it was not widely prescribed in Scotland.
The menopause champion demonstrated that GPs were warned against prescribing it on cost grounds.
The Scottish Medicines Consortium (SMC), which approves drugs for use in Scotland, rejected the progesterone drug Utrogestan for general use in 2009.
On Tuesday, the Scottish government said it would welcome a resubmission from the French manufacturer Besins, to the SMC.
It added that where licensed medicines were not routinely available on the NHS because they had not been approved by the SMC, clinicians could still prescribe them on an case-by-case basis.
The number of prescriptions for HRT across the UK has risen by about a third in the past few years, with about 400,000 prescriptions issued in Scotland in 2020.
But supply of some of the drugs has failed to keep up with demand
The UK government announced last week that it was rationing supplies and appointed a new HRT tsar to help solve the crisis.
In her Channel Four documentary Sex, Mind and Menopause, external, broadcast on Monday, Ms McCall explored the latest medical science on the menopause and perimenopause.
The 54-year-old spoke to doctors about the benefits of Utrogestan.

What is Utrogestan?
It is progesterone which, along with oestrogen. is one of the hormones used in HRT for women experiencing menopausal symptoms.
Most symptoms are due to women becoming low in oestrogen when their ovaries stop working but without progesterone there can be a thickening in the lining of the womb, which can cause dangerous health effects.
Many women take a combined synthetic oestrogen and progesterone HRT but some prefer to take them separately.
Utrogestan is what is called "body identical". It is derived from plants that are biochemically identical to the progesterone hormone produced by the ovaries.
According to The Menopause Charity, it is better tolerated and has a lower risk of breast cancer compared with synthetic progestogens.

'I had to go to a specialist consultant'
By BBC Scotland's Laura Maxwell, presenter of Good Morning Scotland
I was just 41 when I was diagnosed with early menopause seven years ago. That's more than decade earlier than the average woman in the UK - and so I was advised to begin HRT as soon as possible to protect against osteoporosis (fragile bones) in later life.
As can often be the way, hormone-related medications can be a bit trial-and-error, and over the following years I learned to keep a record of how it was affecting me - both mentally and physically.
Several versions of HRT, and a raft of adverse side effects later, I began to research alternatives - if I was going to be on this medication for years, I wanted to ensure it didn't make me feel worse.
Micronised progesterone - or Utrogestan - kept popping up in searches for easier to tolerate HRT. When I asked my GP in Renfrewshire if I could try it, alongside oestrogen gel, they were perfectly straightforward - it wasn't what they usually prescribed, and they'd rather refer me to a menopause clinic.
The consultant agreed it would be a good combination of treatments for me, and I've received repeat NHS prescriptions ever since. It works for me.

Postcode lottery
In her documentary, McCall revealed that being prescribed Utrogestan was a postcode lottery.
She spoke to Kilmarnock GP Dr Helen Smith who described it as "a good safe medicine to use".
But when she tried to prescribe it, her NHS computer system flashed a warning that the drug had not been approved and that an alternative should be considered.
It was claimed that Utrogestan represented a cost of £18 per year, per woman, more than the next less expensive drug.

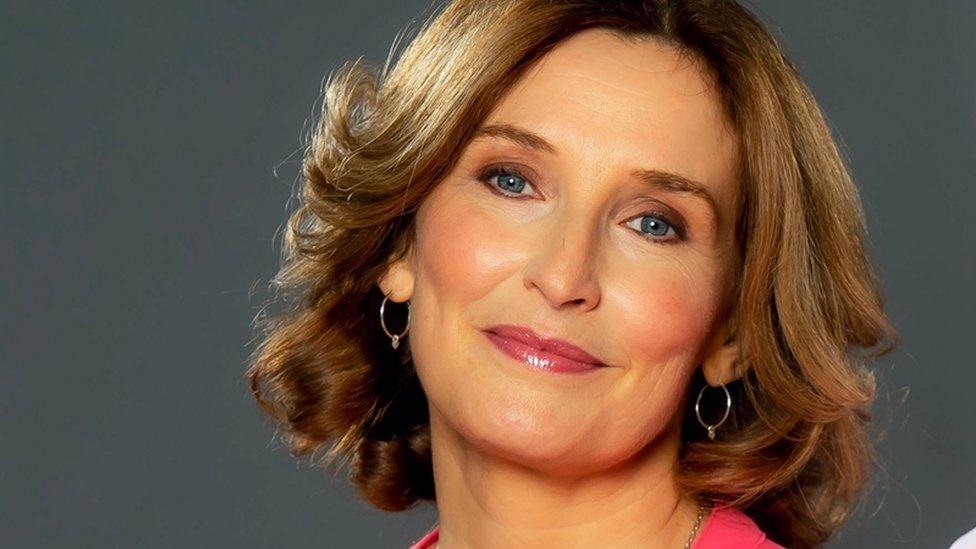
Caroline Phipps-Urch has had to pay privately for her prescription but fears for those who are not in a position to do the same
In 2021, Edinburgh woman Caroline Phipps-Urch started a petition, external to try to influence NHS Lothian to make Utrogestan prescribable.
After researching the best HRT for her own personal circumstances, she went to her GP only to be told she could not get Utrogestan the NHS and would have to pay privately for an appointment as well as the prescription.
Ms Phipps-Urch, who is one half of "The Menopause Sisters" along with GP Dr Claire Phipps on UK Health Radio, told BBC Scotland: "I see this as good news. Although the SMC has not approved it for Scotland, some health boards have it on their formulary and GPs can prescribe it."
She said she was only aware of one woman at her GP surgery in NHS Lothian who had been successful with getting the drug through the Pacs process, which allows approved drugs to be prescribed even if they are not on the GPs list.
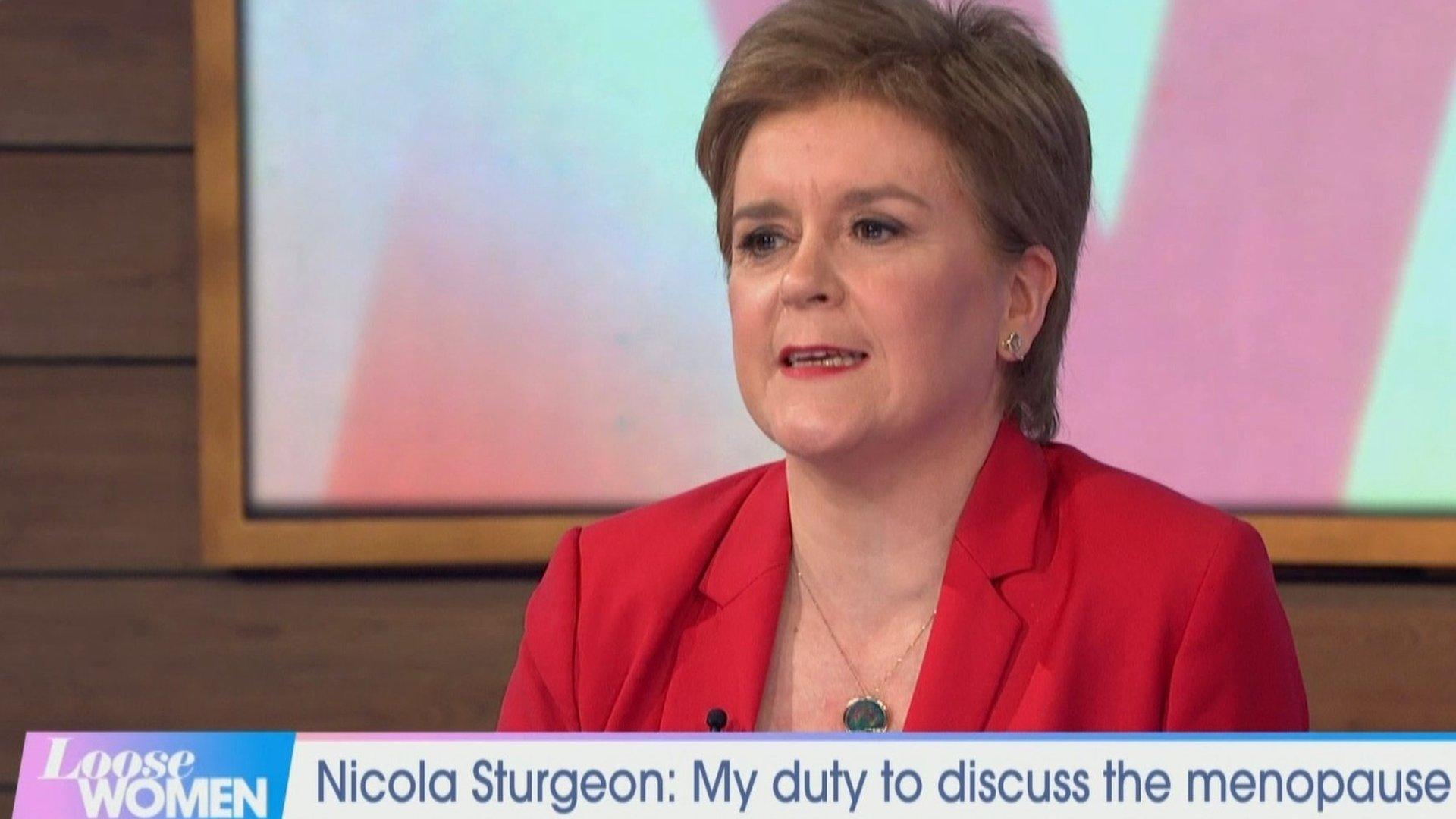
Nicola Sturgeon talked about the menopause during an interview on ITV's Loose Women programme
The SMC said that in 2009 its committee was not satisfied with the evidence the company behind Utrogestan presented on its value for money to NHS Scotland.
But it added that since that advice was issued, another company now owned the rights to the medicine.
A spokeswoman said: "It has been urged to make a resubmission so that we can assess the evidence and provide updated advice to NHS Scotland."
She added: "The only alternative is the mirena coil which uses a synthetic progestogen. It is cheaper but a lot of women don't want that.
"NICE guidelines say it should be an individual approach for each woman. This is about giving a woman choices and about inequality."
The developments came just two weeks after First Minister Nicola Sturgeon revealed she was "in the foothills" of the menopause.
Speaking to ITV's Loose Women programme, Ms Sturgeon said she hoped addressing the issue would help tackle the stigma around the subject.
On her own experience, the 51-year-old said: "Obviously I'm in the foothills of it. I've been quite anxious about - given the public nature of my job - how I am going to cope with the impact of that, what's it going to be like."
She said she hoped women in a similar position would benefit from hearing about her experience.
The UK Department of Health and Social Care said demand for HRT had risen by 38% in the past seven years, but most of the 70 products available remained in good supply.
- Published1 May 2022

- Published20 April 2022
- Published20 April 2022