Social care pay gap could be 'catastrophic'
- Published
Jaclyn Daly said she does not earn enough working as a carer to support herself while studying
Social care providers in Scotland have said a growing pay gap between NHS and social care staff must be addressed to avoid catastrophe in the sector.
They have warned they cannot pay enough to attract staff to look after Scotland's growing elderly population and keep them out of hospital.
Providers said nurses and carers were leaving for better wages in the NHS and overseas.
Scottish ministers said their workforce strategy would address the challenges.
At the Erskine care home in Edinburgh, Jaclyn Daly from Canberra, Australia works as a care assistant while she studies nursing.
Cathy Combe, a resident at the home for military veterans and their spouses, says the staff are all lovely.
"They do everything for you, and you never have to worry about a thing," the 89-year-old says.
"Before my husband passed on, they were very kind with him. I thought I would have to move when my husband died. But they said, no, you are a widow of the regiment - and that's how I'm still here now."
'NHS wages are better'
Jaclyn is a fourth-year student nurse, who works as a care assistant, but also picks up bank shifts in the NHS.
"It's hard because when you work in the NHS, the wages are a little bit better, depending on the type of shifts, and the holiday pay that you get compared to here," she says.
"But you've got uncertainty with it. You're not familiar with the area that you might be working in, and you don't know your residents."
She says that in the social care sector "continuity of care is really important".
"It's the little nuances of each resident. It's knowing how they like their tea or their coffee or, for example, a resident who likes to brush his teeth after breakfast."

Ian Cumming, who runs the Erskine care home charity, says staff deserve to be rewarded for the skills they bring
Independent companies and charities like Erskine are paid by local authorities to take in residents whose means fall below the threshold to self-fund their own care, under the National Care Home Contract.
It stipulates that care staff should receive the real Living Wage - £10.90 an hour, as of 1 April.
But Ian Cumming, who runs Erskine, says this is well below the rate paid to equivalent staff in the NHS and other care homes that are council-run.
"The NHS and local authority equivalent is 21% higher, moving towards 24% higher [after pay negotiations]," he says.
"Ultimately that means £5,000 a year more if you work in the NHS, and that's before you start talking about sick pay, pensions, and additional pay at weekends."
'Really skewed labour market'
He says care providers cannot compete on that level.
"We try our very best to make up that shortfall through fundraising," he says.
"People are at the very core of everything we do and our staff deserve to be rewarded for the unique skills that they bring."
Demand for staff is strong, with a whole time equivalent (WTE) vacancy rate for NHS nurses (and midwives) at 8.2% as of 31 Dec 2022.
But data published by the Care Inspectorate in November showed the WTE vacancy rate for nursing staff in care homes for older people stood at 16.2%.
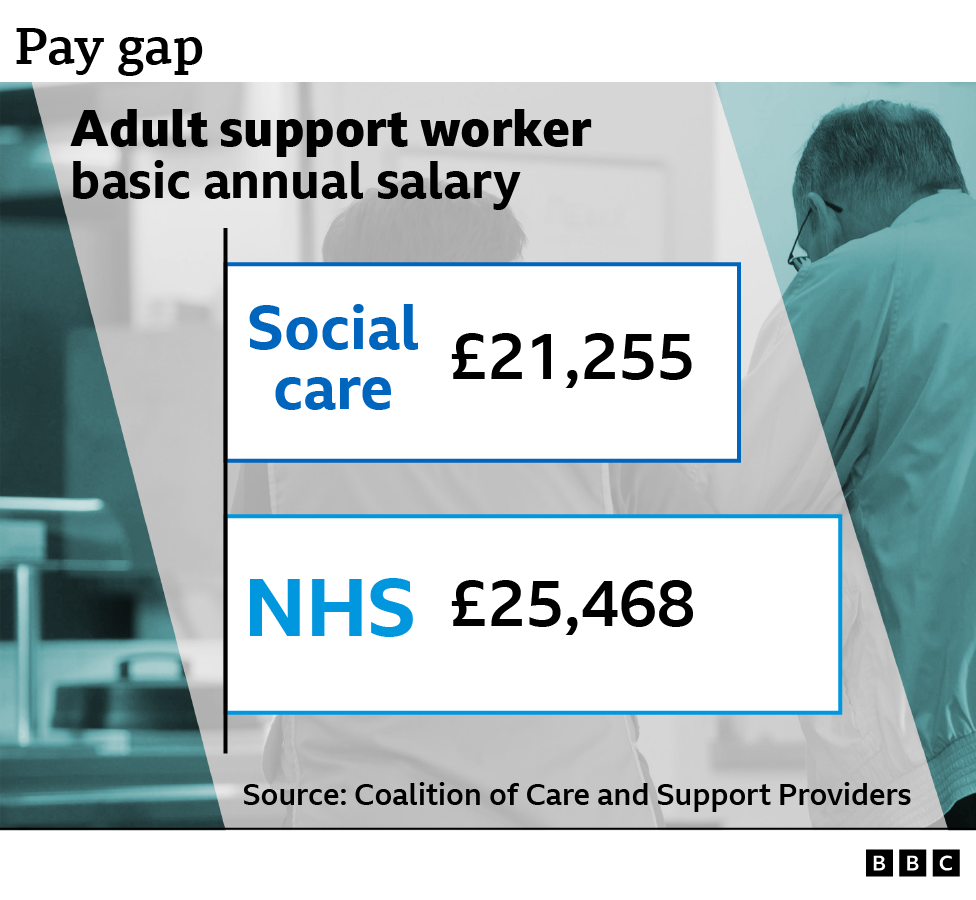
According to the Coalition of Care and Support Providers in Scotland (CCPS), the current basic gross salary funded by the Scottish government for an adult support worker is £21,255.
In the NHS, someone doing the equivalent job is now on £25,468, without taking account of better pensions and other benefits.
Rachel Cackett, chief executive officer of the CCPC, says failure to act now to address the pay gap could be "pretty catastrophic".
She thinks NHS staff deserve pay rises, but warns of knock-on effects.
"The more pay rises we see going into the NHS, the bigger the disparity in pay between a support worker in social care, doing equivalent work to a support worker in the NHS. And that means we've got this really skewed labour market in Scotland, where it's really hard to hold on to people."
When Jaclyn, 32, is fully qualified, she'll face a choice about which path to take.
"There is a pay gap and that will come into it. I'm at a fortunate stage with my life that I don't have many bills, I don't have family, so for me, I can go more where my heart leads a little bit," she says.
"But I do know for some of the older girls on my course that have children and more responsibilities, that they will probably follow the money.
"I guess I'm really privileged in the fact that I'm from Australia and I've got that flexibility to go home. I've got nurses in my family in Australia and they're all telling me to go back, particularly because there has been a whole social care reform in the last couple of years."
"So it's a difficult decision. Scotland has trained me. But you do hear people are going overseas to places like Australia for better conditions and better pay."

Care worker Cristita with Erskine resident Muriel
Another resident at the Erskine care home, Muriel, says it's important to have staff that know you well.
"My eyes have been opened to what old age is all about," she says. "It has its moments but it's not wonderful. I have Parkinsons and it's getting worse."
Ian Cumming believes good care for residents such as 79-year-old Muriel can ultimately reduce strain on the NHS. He says Erskine has a higher bill for staff, because they employ a variety of specialists.
"We are layering on advanced nurse practitioners, speech and language therapists, physiotherapists, all on site to help people to live well and keep out of hospital. Not every care provider can do that, and none of it's funded," he says.
The financial climate means Erskine is running an unsustainable model.
"We spend £2,000 a week in terms of the staffing ratios, the specialist roles we've got, and the number of activities we have.
"We can do it because we're a charity, but this year I'm running £6m in the red in order to maintain that and I will be taking that from our reserves," Ian adds.
Calls for 'parity of pay' plan
Rachel Cackett says many care providers may be forced to hand back contracts - reducing even further the number of care beds available.
"We need much more laser vision from the Scottish government and pretty much the equivalent of what they're giving to our NHS," she adds.
The CCPS is calling on the new cabinet secretary Michael Matheson to implement an hourly rate of at least £12 an hour for social care staff, and to publish a plan to move towards parity of pay and terms and conditions.
These issues were due to be at the heart of the design of a new National Care Service - but that legislation has been delayed following concerns about its price tag.
A Scottish government spokesman said: "Social care has felt the impact of Brexit on staffing, restrictions due to the pandemic, and increased costs due to energy prices and inflation and we are grateful to all staff and partners who have been working with us to look at solutions.
"Extra government funding has already helped deliver two pay rises for staff in two years and we are currently working on improved terms and conditions.
"Our national workforce strategy looks at how we can plan for, attract, train, employ and nurture our health and social care workforce."
- Published22 March 2023

- Published1 March 2023

- Published27 January 2022
