Angry Birds inspired surgeon's 'game changing' tool
- Published

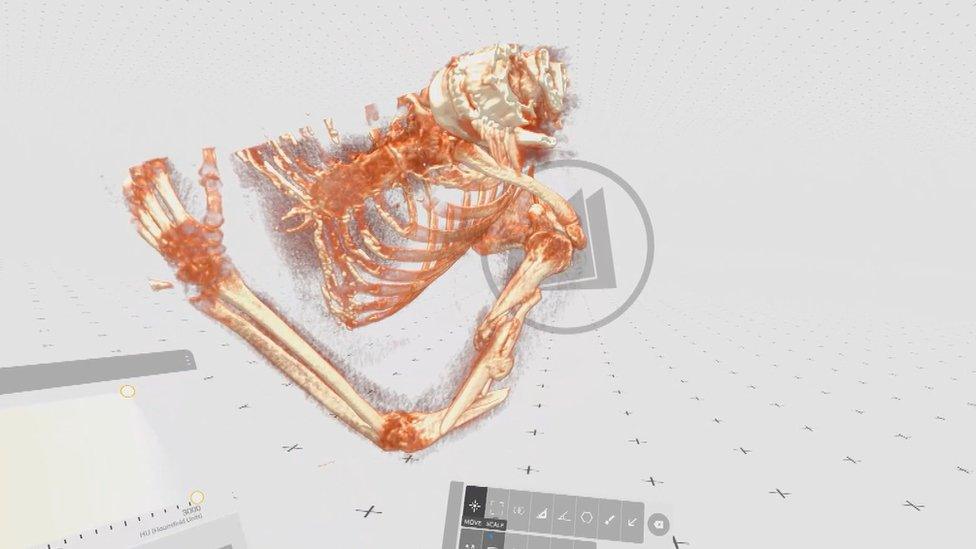
Surgeon David Howie describes the VR technology he is using as a "game changer"
Trauma surgeon David Howie has found a way for virtual reality technology to help repair shattered bones.
The Scot came up with the "game changing" idea after playing a computer game with his daughter.
His team went on to develop a way to rehearse complex procedures outside the operating theatre which has transformed complicated operations.
Surgeons at NHS Lanarkshire now believe the low-cost system has the potential to help other orthopaedic surgeons.

Surgeons can rehearse the surgery before they enter the operating theatre
Mr Howie told BBC Scotland News: "My daughter and I got a VR headset for Christmas and it was great for gaming and playing Angry Birds and things.
"I suddenly thought, hang on, we should be able to view CT scans using this same technology and there must be clever people who have already created the software.
"I looked around and discovered a couple of versions of the software and we chose one to use."
NHS Lanarkshire's IT staff joined in to develop the project and now doctors at University Hospital, Wishaw are using VR headsets to view high-tech 3D images of complex injuries.
It allows them to get a better view and understanding of the fracture, meaning they can plan more precise surgery.
Using software by a company called Medicalholodeck, existing technology was adapted so doctors could use it to see patient's scans and rehearse their surgery in as realistic an environment as possible.
'Smashed up mess'
Mr Howie said: "Once you've used it you realise how effective it is at giving you an understanding of what you are looking at.
"You can clearly see where the fracture is, what the configuration is, all the other little bits of fragments and it gives you a much better idea of where it is broken. And it really helps us plan how we are going to fix it.
"In really complicated ones where there are six or seven different pieces, it is a game changer".

Surgeon Elizabeth Crighton operates on a complex arm break after using VR to plan the procedure
It will not work for all patients but Mr Howie said it could make a big difference in some cases.
"In the small number of really complicated cases where it's a bit of a smashed up mess, it's really nice to get your head around the mess before you start to get your knife around it," he said.
Virtual Reality is already used in surgical training and is increasingly being used to support patients in other areas of healthcare, but this is the first time in Scotland that surgeons have used the technology as part of their pre-operative preparations.
Trauma Surgeon Elizabeth Crighton has a long day in theatre ahead of her. She is operating on a patient who has complex humeral fracture in her upper arm. It has caused nerve weakness meaning she is unable to move her hand.
Surgeon Elizabeth Crighton could see the complex arm fracture from all angles and practice her surgical procedure
Ms Crighton said: "The fracture is broken into lots of small, different pieces that are in all different orientations so with the VR headset we were able to visualise that beforehand which is really useful in planning our operation so we know where the different bits of bone are and how we are going to fix them together.
"You only get one chance at this to fix it perfectly and these complex three dimensional fractures are not very good visualised just on an X-ray so that's where the VR comes in for us."
Mr Howie said companies had developed technology that does the same thing - and probably better.
But this is expensive and requires vast hardware. What NHS Lanarkshire has developed is a cost-effective way that works.
This pilot project cost less than the materials required for two hip operations.
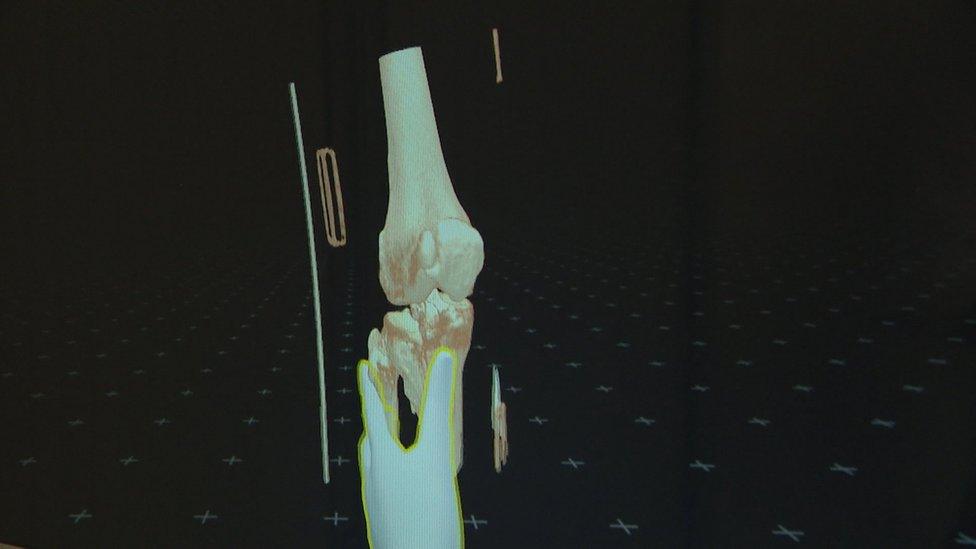
Using the headset, the surgeon can get into the bones and plan the most efficient way to fix them
Staff are collecting data to measure its success. If it does prove cost effective and can improve outcomes and patient experience, there is scope to extend it to other surgeries.
Lyle Boylan, NHS Lanarkshire's E-health transition manager said: "We think it will help to reduce clinical risk because it should speed up operations by giving us a better understanding, before we start these operations, of what is needed.
"We think we can use it for a patient experience point of view as well and actually show people what is happening in an operation in an easy-to-understand way".