My four-year wait to see an NHS dermatologist
- Published

A young woman with a severe skin condition spent almost four years on a waiting list to see an NHS dermatologist in person.
Charlotte Brown, 31, from Edinburgh, was first diagnosed with psoriasis in 2017 and referred for light therapy in 2019.
It wasn't until September this year that she began treatment.
Psoriasis is a chronic condition that causes inflammation on the body that forms flaky patches of skin and scales.
Symptoms range from mild to severe and can have a huge impact on someone's life.
"It's exacerbated by stress, so when you are in that endless cycle of not knowing when you are going to next get treatment it does get frustrating and it can make you feel quite vulnerable, especially because it is a very visible condition," Charlotte told BBC Scotland News.
"If you don't have the time to sit and put creams on, it gets dried out really fast and that's when it starts to break and bleed."

Charlotte Brown waited almost four years to be seen over her psoriasis
Although delays to Charlotte's treatment were exacerbated by Covid, it has not been uncommon in recent years for patients to face long waits to see a dermatologist.
Data released by Public Health Scotland revealed that more that 8,000 people had joined the waiting list for a dermatology outpatient appointment in the three months to June - and that list had grown by more than any other NHS specialty.
It comes as statistics showed that NHS waiting lists in Scotland have grown to a record high, with more than 670,000 names in the queue to see a specialist for non-urgent care in the latest quarter - including more than 500,000 waits for an outpatient appointment.
The Scottish government has a national standard whereby 95% of new outpatients should wait no longer than 12 weeks from referral to being seen.
However, waiting times have been growing since the pandemic with hospitals struggling to free up beds and create additional capacity.
Scottish ministers pledged to spend an additional £100m a year to bring down the longest waits - and there has been a slight reduction in the number of people waiting over two years for an outpatient appointment - but a growing number waited over 18 months for inpatient treatment in hospital.
Cardiology, dermatology and neurology were the specialisms with the highest increase in waits for a new outpatient appointment last year.
Although Charlotte was able to speak with a dermatologist via Whatsapp during her wait, she says the delay to begin treatment and see a consultant in person meant that her condition went from manageable to severe.
She says her psoriasis began with just a couple of small patches on her body, but it has now spread across most of her arms, legs, back and face.
"Sometimes you just want to be out in a bar with your friends and not have people come up and point or ask if it is contagious. You want to be out and about having a normal life," she added.

Karen McLeod did not want to wait any longer to have her lipoma removed
Prof Colin Fleming, a consultant dermatologist at NHS Tayside, told BBC Scotland News it was hard for many dermatology services to "recover lost ground since the pandemic" partly because the services had to concentrate on skin cancer.
"This has meant that many NHS dermatology services have maintained reasonably short waiting times for cancer detection and treatment but many life-altering conditions, such as eczema or psoriasis, now have long waits to be seen," he said.
It is for these life-altering but not life-threatening conditions that some patients are now turning to private health to get treatment for.
In 2020, Karen McLeod noticed a growing lump on her forehead.
After getting referred by her GP to see a dermatologist, Karen was told the lump was a lipoma - a non-cancerous lump that is not typically removed by the NHS.
However, the lump continued to grow until it ran from her hairline down to the middle of her forehead.
"I feel really down about it, looking at my pictures and other people have commented now," she said.
"I always try to hide it, but it really does have a big impact on me."

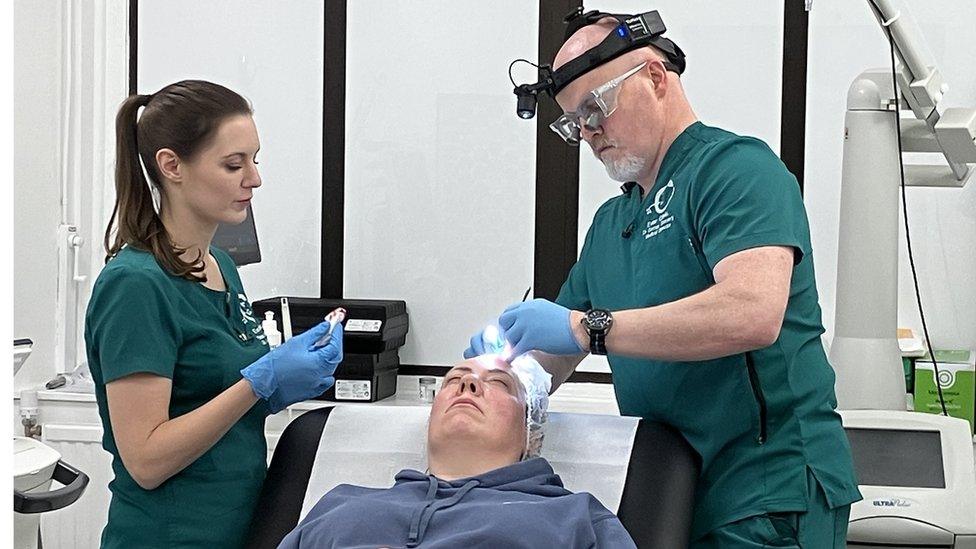
Dr Cormac Convery said skin conditions had a detrimental effect on quality of life
Karen was told it was highly unlikely she could get the lipoma removed on the NHS as it would be considered a cosmetic procedure despite it having a "huge impact" on her daily life.
She felt she had no choice but to pay £800 at a private clinic in Glasgow to get the lump removed.
"I just feel I work hard, I pay my taxes like everybody else, and obviously that contributes to the NHS and it would be nice just to have a wee bit back," she said.
Dr Cormac Convery, who was a GP for over a decade before taking up work at a private clinic in Glasgow, said he increasingly sees patients who have "serious life-changing differences" that they can't get treated on the NHS.
"They withdraw from society, they stop working and it just has a massively detrimental effect on their quality of life and it is more of those people who we end up seeing," he said.
Karen McLeod went private to have a lipoma removed from her forehead
Owners at the Ever Clinic say their service began as more cosmetic-focused, but they quickly pivoted resources as it became clear there was a high demand for minor surgery from patients who couldn't get NHS treatment or faced years-long waits.
The most common treatments include removing lipomas, rhinophymas and moles - procedures which cost £800, £3,495 and £275 respectively.
"Transparency is the critical thing," Dr Convery said.
"Many of our patients have engaged with the NHS and have received some sort of attention but it's just the timely delivery of that care that is not supportive of that patient's need, and when we go to years waiting for that treatment it's just not workable for the average individual."
The Scottish government said there were "unacceptable waits" in some specialities but that it was determined to ensure people receive the treatment they need as soon as possible.
A spokesman said: "The first minister has announced new annual funding of £100m to help reduce inpatient and day-case waiting lists by an estimated 100,000 patients over the next three years.
"We are working with NHS Boards to reduce long waits, which have been exacerbated by the impacts of the global pandemic. This includes targets to address long waits and delivery of the commitments in our £1 billion NHS Recovery Plan to support an increase in inpatient, day-case, and outpatient activity.
"Two National Treatment Centres opened this year in Fife and Highland, with two further centres opening soon in Forth Valley and the Golden Jubilee, providing additional protected capacity for patients across Scotland."