Scotland's NHS cannot meet growing demand, warns watchdog
- Published

Scotland's NHS is unable to meet the growing demand for health services, a spending watchdog has warned.
A review by Audit Scotland said the increased pressure on the NHS was now having a direct impact on patient safety and experience.
The watchdog also claimed there was no "overall vision" for the future of the health service.
Health Secretary Neil Gray said reforms were already under way and he would shortly unveil his vision for the NHS.
The annual report on the state of Scotland's health service highlighted that the NHS was facing soaring costs, patients were waiting longer to be seen and there were not enough staff.
Stephen Boyle, Auditor General for Scotland, said this had "added to the financial pressures on the NHS and, without reform, its longer-term affordability".
He added: "Without change, there is a risk Scotland's NHS will take up an ever-growing chunk of the Scottish budget. And that means less money for other vital public services.
"To deliver effective reform the Scottish government needs to lead on the development of a clear national strategy for health and social care.
"It should include investment in measures that address the causes of ill-health, reducing long-term demand on the NHS."
NHS performance
The twin challenges of recovering from the Covid pandemic and increasing demand was impacting the service patients receive, according to the Audit Scotland report.
It pointed out only three out of eight key Scottish government waiting times standards had been met at a national level in any quarter in the last five years.
The number of ongoing outpatient waits last year was 525,654, up 10.5% on 2022 and up from 319,356 in 2019.

Audit Scotland said Scottish ministers' commitment to reduce waiting lists and waiting times in 2023/24 was "unlikely" to be met on current progress.
The number of people whose discharge from hospital had been delayed was still higher than before the Covid pandemic.

Elsewhere in the NHS, ambulance crews were, on average, spending 23 minutes longer at hospital for every patient conveyed there compared with before the pandemic.
The watchdog's report stated that the NHS, and its workforce, was "unable to meet the growing demand for health services".
Patient safety
Audit Scotland said the increased demand and performance problems were having a "direct impact on patient safety and experience".
The watchdog highlighted that Healthcare Improvement Scotland, the body which carries out safety inspections in hospitals, had highlighted some serious concerns to boards in the last year.
These concerns include overcrowding in emergency wards, lack of privacy for patients and buildings in poor condition.

A number of Healthcare Improvement Scotland's concerns also related to workforce issues such as high levels of agency staffing and staff feeling exhausted or unable to provide safe care.
Audit Scotland also said some staff still lacked trust in processes for raising safety concerns within health boards.
The financial outlook
Health is the single largest area of public spending and is projected to take up an increasing share of the Scottish government's budget in the coming years.
In the last decade, Audit Scotland said direct health spending had increased by 21% in real terms but the financial outlook for the NHS remained challenging.
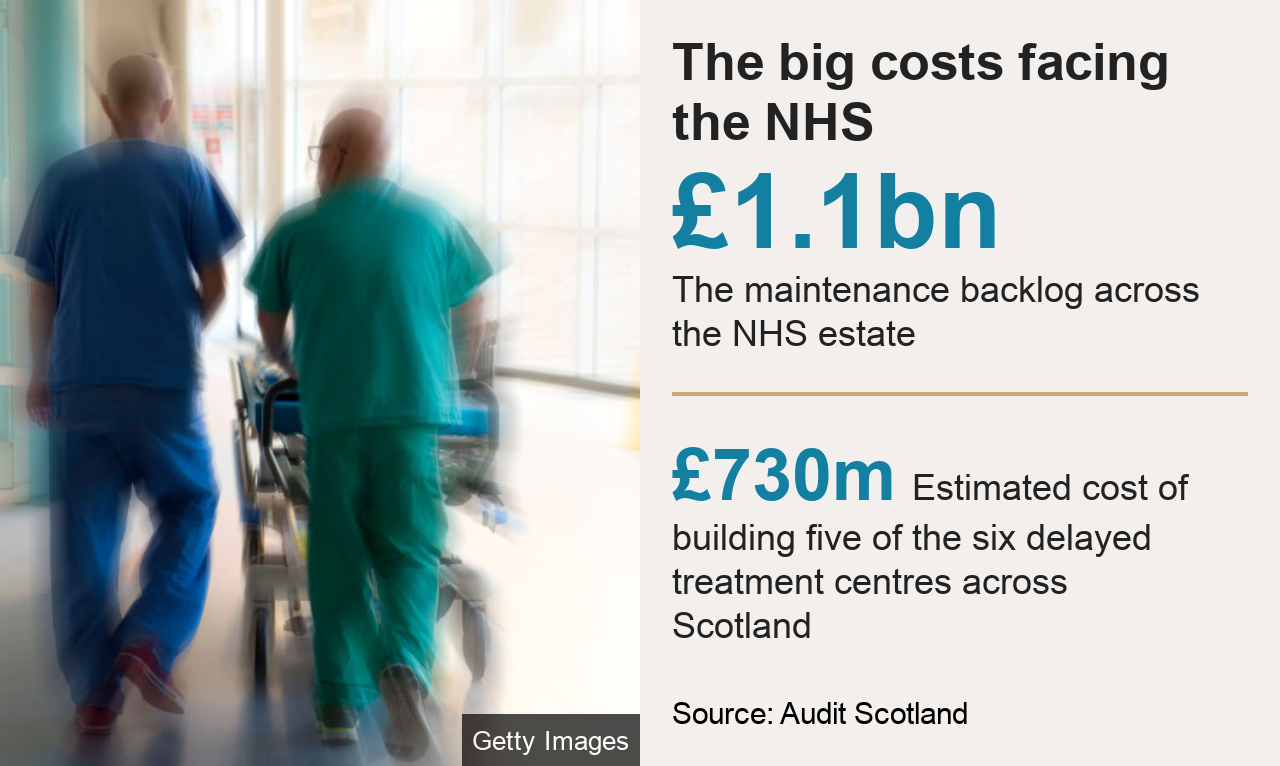
Spending on building new hospitals, surgeries and a network of treatment centres across Scotland has been put on hold as a result of budget pressures.
Audit Scotland said this squeeze on the NHS capital funding meant this budget was now "unlikely to keep pace with increasing costs and existing commitments related to delivering national treatment centres".
It also suggested that the current funding available for maintenance was "unlikely to be sufficient".
In 2022/23, five health boards needed Scottish government bailouts to balance their books and seven health authorities are on track to need this again in the current financial year.
Increased costs are driving the financial pressures facing the NHS, with energy costs alone up 21% in the last year.
The biggest outlay was staff.
A pay hike for the 180,000 NHS employees in Scotland took the wage bill for 2022/23 up to £9.8bn, which Audit Scotland said was 23.5% higher than five years ago.
The number of staff employed in the NHS has increased over the last five years, however the number of vacancies has also increased.
This is partly being dealt with by using temporary workers.
The total NHS spend on agency staff in 2022/23 was £381.8m, up 27.5% on the previous year.

'We are in dire straits'

John died in 2022
Trish Nolan's husband John was admitted to Victoria Hospital in Kirkcaldy in May 2022 as a planned emergency admission while suffering from bladder cancer.
He was bleeding profusely, in "terrible pain" and was unable to control his bladder or bowel.
However, on arrival, he was directed to a room that had what Trish described as hard, table-like bed.
Trish waited by his side for almost five hours before walking out of the room, described by one paramedic as a "cupboard," and hitting a crash button to receive some attention.
Trish said: "John was very distressed. He had no cannula in place, there was no patient buzzer. If I had not been there, I believe John would have died in that room.
"His veins had collapsed, he was confused and delirious and there was blood everywhere.
"When he was admitted, I started to feel really scared for him. On that day, I would say that was when the safety issues became very apparent."
John died at a hospice in Dunfermline about a month later, having developed sepsis during his three-week stay at the hospital.
Trish said he felt safer at home and "abandoned" while at the hospital.
She said: "It was a man who was dying of cancer, if that is not a priority, we are in dire straits."
NHS Fife's director of nursing, Janette Keenan, said: "We are unable to comment on the specifics of Mr Nolan's care for reasons of confidentiality. We can confirm, however, that we continue to meet with Mrs Nolan to discuss her concerns in detail and to learn from the family's experience."

'Reform alone will not save our NHS'
Mr Gray, the Scottish government's health secretary, told the BBC's Good Morning Scotland that the NHS was in a "position of recovery" following the Covid-19 pandemic, and that he would soon present his plans for reform to the service.
He stated that he would be looking to "invest in the workforce, invest in the service to ensure we see continued progress in that recovery" and added that he would consider private investment in the NHS, in a similar way to the mutual investment model that has been used in Wales.
Mr Gray also refuted any concerns that NHS Scotland services are not safe for patients.
He said: "Of course in an organisation of its size, with 160,000 staff, there are going to be pressures, there are going to be elements where there are mistakes made, but I am incredibly proud of the work that our staff do to provide incredible care."
Scottish Conservative health spokesman Dr Sandesh Gulhane MSP said the "utterly damning report exposes the monumental failings of the SNP's management of Scotland's NHS".
He added: "As well as having no clear vision for our health service, SNP incompetence has meant there is now no money to progress desperately needed new healthcare facilities across the country".
Prof Andrew Elder, president of the Royal College of Physicians of Edinburgh, said: "Reform alone, in the absence of increased funding, will not save our NHS.
"At the same time, it is legitimate to ask whether we can afford to provide every treatment available, free of charge and at the point of access. If we cannot - which is plausible given the huge increases in medical treatments available - how should we decide what we can provide?".
Dr Iain Kennedy, chairman of the British Medical Association Scotland, said the report was "staggeringly bleak and paints a picture of a health service in crisis, without a plan to address it".
He said: "The report confirms the NHS in Scotland, and its workforce, is simply unable to meet the growing demand for health services of our population."
The Royal College of Nursing Scotland said unacceptable and unsafe working conditions were being normalised, and that nursing staff were burnt out.

For some time, doctors have been warning that lives are being lost because the NHS is not working properly. The Auditor General - appointed to check public money is well spent - would normally be expected to use more conservative language.
But this year he has chosen to state for the first time that the health service is not just struggling, but incapable of meeting the demand for care - and that patients are at risk as a result.
The NHS won't just keel over, but if it continues to be "unable" to meet demand, then other things will have to give - whether that is access to new medicines or buying innovative equipment - and people will have to wait even longer for the care they desperately need.
The government says it is committed to free access to healthcare but a growing number of respected medical bodies are calling for a frank conversation with the public about whether the NHS can afford to provide every treatment free of charge.
Related topics
- Published28 November 2023

- Published18 May 2023

- Published19 February 2024

- Published20 February 2023

