High risk prostate cancer death 'cut with radiation'
- Published
Some men suffered "mild" side effects
Deaths from high-risk prostate cancer can be cut by giving men radiation treatment as well as hormonal therapy, research by Cardiff University has shown.
A trial of 1,200 men with prostate cancer spread from where it started to nearby tissue or lymph nodes found additional radiotherapy cut deaths by 43%.
All the men received hormone therapy.
The interim results were presented to a cancer experts conference in Liverpool.
Trial leader Prof Malcolm Mason called the findings "exciting".
The trial found that the additional radiotherapy cut deaths by 43% after seven years.
Early results showed that 79% of men who had hormone therapy alone were alive seven years later compared with 90% who received radiotherapy and hormone drugs.
Hormone treatments can work well but some men stop responding to them after a few years.
Prof Mason said he hoped men would be offered radiotherapy following the findings of his research.
The results follow a trial over 11 years.
Prof Mason added: "These exciting results clearly show how radiotherapy increases survival for men with this type of prostate cancer.
"Currently, we estimate that around 40% of men like those in the trial are given radiotherapy in the UK, and we hope that, thanks to these results, more men will now be offered this important option."
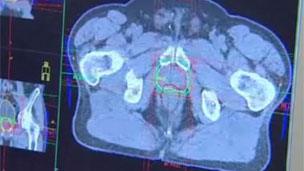
The men who received radiotherapy were treated five days a week for between six or seven weeks as outpatients.
Fresh hope
Some men suffered "mild" side effects including discomfort, the need to urinate frequently or diarrhoea.
However, radiotherapy has long-term effects that may not be seen for three or four years, including a risk of impotency.
But charity Cancer Research UK, ahead of the National Cancer Research Institute conference, welcomed the findings.
Kate Law, director of clinical research at Cancer Research UK, said: "This trial offers fresh hope to thousands of men with prostate cancer, preventing hundreds of deaths every year.
"Radiotherapy is sometimes an overlooked form of treatment, but this trial shows how vital it can be."
- Published26 August 2010
- Published10 September 2010