Every child with asthma in Wales 'needs plan'
- Published

Every child diagnosed with asthma should have an action plan for their care, a senior doctor has said.
Dr Iolo Doull, paediatric respiratory consultant at Cardiff's University Hospital of Wales, said guidelines from health watchdog NICE should be implemented consistently.
The condition is so common, concerns are being raised people have forgotten asthma can kill.
In Wales, approximately two children a year die as a result of the condition.
Many more need hospital treatment.
Asthma UK estimates 59,000 children aged 15 and under in Wales have asthma - an average of three in every classroom.
Wales and the UK have the highest asthma mortality rate in Europe, five times higher than countries such as Sweden, Portugal, Germany and Italy.
'More training'
In 2014, the National Review of Asthma Deaths, published by the Royal College of Physicians, highlighted that in the last decade, despite advances in medication and improved guidelines, the asthma death toll in Wales and the UK remained level.
It cited complacency as a major problem and identified the need for more training, monitoring and education.
Dr Doull said there was very little information about asthma plans in Wales.
He said: "We know that within England, where you have quite good data on primary care trusts, the rate of asthma hospital admissions varies 19-fold.
"Socio-economic factors alone did not explain the huge variation, which suggests that variations in practice affect the rate of hospitalisations. It's almost certainly the same in Wales."

'Take asthma more seriously'

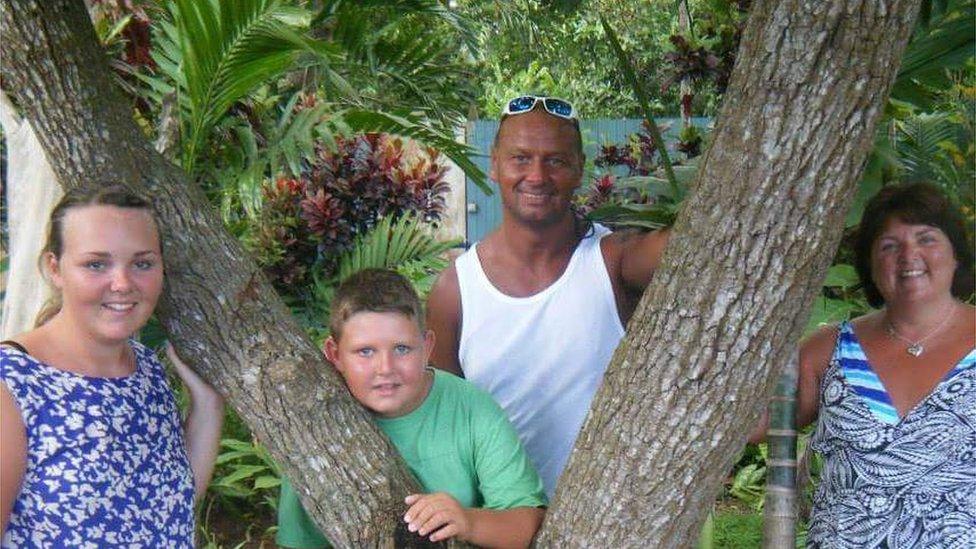
Geraint Richards suffered brain damage after having an asthma attack
Chris and Julie Richards live near Bridgend and are the parents of 13-year-old Geraint.
He suffered from asthma from a very early age, but it was controlled using a preventer inhaler as well as a reliever inhaler.
He led a normal active life until two years ago when he had an asthma attack.
Unfortunately, he did not respond to treatment in hospital and the attack led to a cardiac arrest which almost killed him and left him with severe brain damage.
Prior to the attack, Geraint did not have an asthma action plan and the family now believe he was using his reliever inhaler excessively.
The family are backing calls for asthma action plans, more monitoring to be standard practice and for the condition to be taken more seriously.

Dr Doull told BBC Radio Wales programme Eye On Wales: "Asthma is the commonest chronic condition in childhood. It can significantly affect children and families' everyday lives. It can lead to death. It's a major problem and it should be taken seriously.
"It's frightening and it's incumbent upon us to see if we can prevent these deaths.
"I think that every patient with asthma should have an asthma action plan - you're giving the patient a clear set of instructions about what to do and when to seek medical help."
Dr Doull is the paediatric lead on the NHS Wales-led Respiratory Health Implementation Group. He is chairing the team tasked with developing guidance on how to improve services for children with asthma in Wales which will report its findings this summer.
"Using your reliever inhaler excessively is a warning sign," he said.
"All the guidance and all the evidence suggest that children and adults should be regularly monitored and there should be a formal undertaking of a review once a year.
"That does happen at present, but I think there could be improvements in the fine tuning of that."
One country which drastically reduced asthma-related health problems in the last decade is Finland.
Dr Tari Haahtela, from Helsinki teaching university, told the programme that it was a combination of earlier diagnosis and treatment and improved guidance on self-management.
"We have achieved a zero asthma mortality rate under the age of 40. We have cut hospital emergency visits as a result of asthma by 50-60%.
"Our slogan is to hit early and hit hard. Every asthma death is an accident and should not happen."
- Published6 April 2016

- Published2 November 2015

- Published28 January 2015
- Published20 December 2014

- Published6 May 2014
- Published6 May 2014
