Hospital workforce crisis 'looming' - Royal College of Physicians
- Published

Hospital doctors in Wales have warned of a "looming crisis" over workload and recruitment, adding to concerns about pressures already made by GPs.
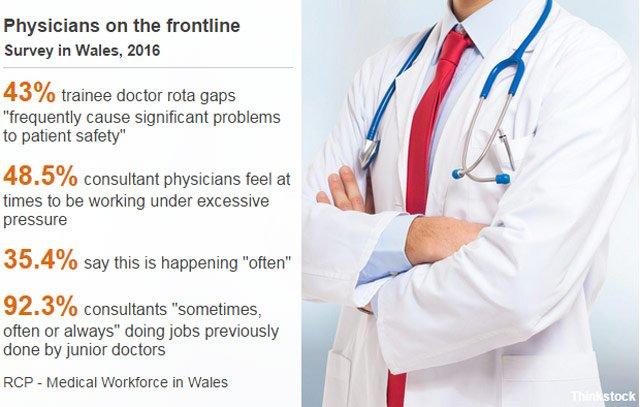
The Royal College of Physicians found 43% of consultants believe rota gaps among junior doctors cause "significant problems" to patient safety.
Meanwhile, 40% of consultant physician vacancies could not be filled.
"In most cases, this was because there were literally no applicants," said Dr Alan Rees, RCP Wales vice president.
The concerns in hospitals follow issues involving a shortage of GPs and a campaign to get doctors to train and work in Wales.
"The NHS recruitment crisis in Wales is getting worse, and is not confined to primary care," said Dr Rees.
This is the first time the RCP has compiled Wales-only figures on the workforce in hospitals.
The findings of a new survey of consultants - and core medical trainees (CMTs) - coincide with a conference in Cardiff.
Consultant physicians are senior doctors who look after everything which is not surgical in the hospital - and that includes 30 different specialisms, acute admissions and outpatient clinics.
The CMTs are qualified junior doctors who have already been through medical school and completed their first two years as trainees.
They do the day-to-day ward rounds and look after patients while on rotations in different specialities over a further two year training period.
The report found:
NHS Wales was unable to fill 39.8% of the consultant physician posts it advertised in 2015. This was even higher for in-demand roles focused on caring for acutely ill and older people.
A third of the 218 CMT doctor posts in Welsh hospitals were vacant in August 2016.
Almost two-thirds of CMTs say they are "sometimes, often or always" working under excessive pressure.
Almost half of the consultant physicians say that there are times when they feel as though they are working under excessive pressure. 35.4% are saying that this happens often.
17% of CMTs have considered leaving the profession in the last year.

WHAT JUNIOR DOCTORS SAY

Dr Charlie Williams and Dr Richard Gilpin are qualified junior doctors
Dr Richard Gilpin, 33, qualified as a doctor six years ago and his current rotation is at Nevill Hall Hospital in Abergavenny, the 12th hospital he has worked at in his career so far.
"We're used to working long hours, so a typical shift is 13 hours and it's not unusual to work a couple of hours after that. And to spend that time, working as hard as we can, missing food and toilet breaks and after that time having 15 to 20 patients still waiting to see a doctor because of rota gaps, that's a very difficult thing to come home from.
"And that's tied in with morale - the idea you want to finish the working day knowing you've done a good job."
Dr Charlie Williams, 28, qualified three years ago and is currently at Morriston Hospital in Swansea on her rotation as a core medical trainee.
"I don't know anyone who's routinely not working longer hours than they should be. When you're on a rota that's very thin there's no wriggle room, if someone's off sick or a car breaks down, you end up having to cover the extra work. You do get quite a lot of phone calls and pressure to fill those shifts.
Dr Richard Gilpin explains the ups and downs of being a junior doctor
"From a training point of view, if you want to learn how to run an outpatient clinic or learn some of the management or educational bits that consultants do, you can only do that if there's enough cover for your ward and you know your patients are looked after.
"When there is no cover, that [training opportunity] never happens. You have this conflict because you need to be able to do these things to progress your career, they're not optional. You then have to square that with whether you can leave the patients; leave the ward.
"It adds an extra layer of pressure and it also makes it less flexible. If you want leave for example - I've got a friend getting married on a Sunday in July, I'm not sure I can go with that much notice because I don't know if there will be a doctor to cover: that's the priority. When you can't plan over those things, it's difficult for your family or to explain to people you know."
Both love their jobs and are keen to stress they find them very rewarding and interesting.
These junior doctors' frustrations are with the rota gaps - not unique to Wales - but also with IT and technology systems inside hospitals, especially having to move between different health boards every six months.
Dr Gilpin said: "There's a joke in medicine that the most important thing you have to learn as a doctor in your first month is how to fix the printer.
"When you've spent half an hour trying to fix the fax machine so you can send a referral off - I could have spent that time talking with a patient's family."
Dr Williams added: "We've got people coming in half an hour early to make up the patient list and then find a printer that works, because you need to have it ready to go or you're holding up the rest of the clinical team".

The RCP makes 30 recommendations set against what it sees as complex challenges, including a rising and ageing population and the need to serve large rural parts of Wales as well as urban areas.
It sets out examples of good practice, particularly in how healthcare needs to go beyond hospital walls.
The organisation also wants more Welsh students to study medicine in Wales, increasing the likelihood of them staying on to work here.
Dr Rees said numbers were now "as low as 10%" of students in medical school in Wales being from Wales.
He added that a "bold, strategic step" was needed and a "really ambitious, long term vision", not more quick fixes.
The Welsh Government said it would consider the report but it was important to recognise how demand was growing.
"In order to address the challenges this poses, health boards have been working hard to recruit more staff, including consultants," said a spokesperson.
"As a result there are more frontline staff working for NHS Wales than ever before. We will continue to support health boards to recruit staff, including doctors, through our 'train, work, live' campaign."
Conservative health spokeswoman Angela Burns AM called on ministers to introduce long-term workforce planning and to bring forward a "fresh recruitment plan".
"This should involve contracting newly trained doctors for a number of years in return for training bursaries, as well as establishing a pilot of financial incentives to attract doctors in shortage specialities and understaffed areas to work in Wales," she said.
- Published20 October 2016

- Published8 September 2016

- Published3 August 2016

- Published2 June 2015

- Published2 December 2010
- Published2 June 2015