HPV in Wales: 'Make vaccine available to all on NHS'
- Published

Vaccination for a cancer-causing infection should be universally available on the Welsh NHS, campaigners have said.
Girls aged 12-13 and gay men of 16-45 are vaccinated against Human Papilloma Virus (HPV) in Wales.
But AM Angela Burns said it was an age and gender "lottery" which should end.
The Welsh Government said there were "no plans" to extend vaccination to adolescent boys, based on independent advice.
It comes after the UK's Joint Committee on Vaccination and Immunisation (JCVI) found on Wednesday there was little evidence to justify treating boys too - a decision which has been fiercely criticised.
This initial recommendation by JCVI will now be subject to a public consultation and a final decision will be made in October.
Angela Burns, the Welsh Conservatives health spokeswoman, said she was "deeply disappointed" by the decision of the JCVI, which advises UK health departments on immunisation.
"Men and women are looking to the Welsh Government to live up to its devolved responsibilities by pioneering a change that will see equality of protection for men and women from HPV," she added.
"I do not believe we should have a... lottery based on gender specifics."
The vaccine was made available to girls in 2008, external as a protection against cervical cancer, with the programme opened up to adult gay men under 45 earlier this year.
The vaccine is available privately but can cost up to £500.

Maria Dullaghan believes she may not have had "full-on cervical cancer" if she had been given the vaccine
'Not just girls'
Maria Dullaghan, 32, of Haverfordwest, Pembrokeshire, who went to school before the vaccine was rolled out, was diagnosed with cervical cancer aged 25.
She said, had she been given the vaccine, she may not have had "full-on cervical cancer" and may have avoided a hysterectomy, radiotherapy and chemotherapy.
Ms Dullaghan now hopes her 15-year-old son, Connor, will be immunised.
"I would love for him to have the vaccine, I have looked into having it done privately, but at a cost of around £500, I'm not in a position to be able to afford that.
"It's not just girls that can get the HPV virus, it can be on everybody. Most people they reckon will get it in their lifetime but symptoms won't show and their body will just get rid of it.
"I think, having boys immunised as well could have a really big effect on the number of girls that then catch this virus, that can lead to cervical cancer."

The virus has been implicated in a growing numbers of cancers in men - particularly in the head and neck.
Dr Mererid Evans, consultant clinical oncologist at Velindre Hospital in Cardiff, said research showed the HPV caused cancers in the oropharynx, which is within the head, neck, tonsils, tongue and throat, as well as other cancers in men, such as anal cancer and penile cancer.
She said data showed rates of oropharyngeal cancer had trebled in Wales over the past 15 years.
"This is a real public health issue - men are being affected, we're treating more and more of them with surgery, chemotherapy and radiotherapy and it's important that we try and prevent these cancers happening in the first instance," she said.
Robert Music, chief executive of Jo's Cervical Cancer Trust, said extending vaccination to boys presented an opportunity to save lives.
"HPV does not just cause cervical cancer. It is also responsible for other cancers that affect both men and women and this decision could have resulted in increased protection against this devastating disease for boys and girls," he said.
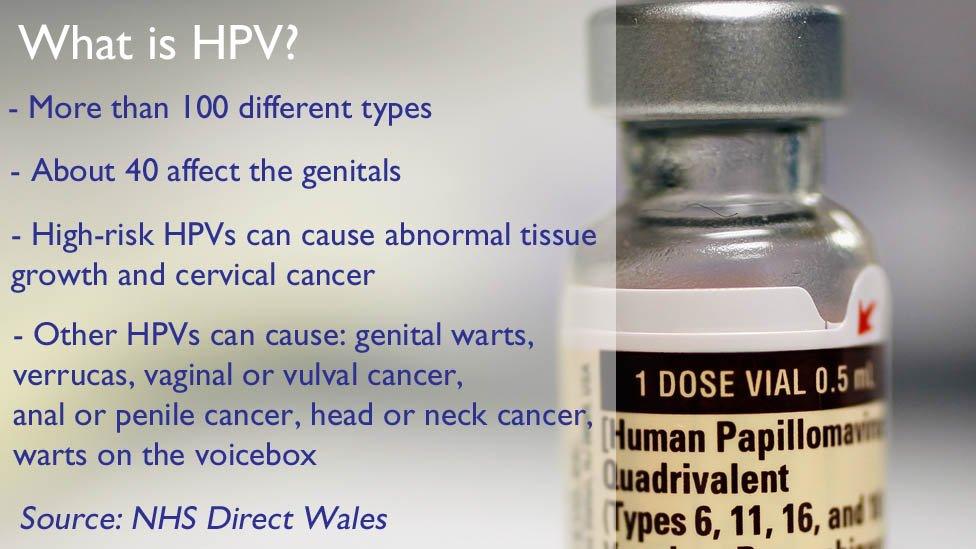

HPV is common, with about 80% of people having it at some point.
It can be temporary and most of the time the body is able to fight it, but in some cases it leads to cancer.
Other strains of HPV cause sexually transmitted infections, such as genital warts.
A Welsh Government spokesman said: "In line with the JCVI's recommendations, there are no plans to extend the HPV vaccine programme to cover adolescent boys in Wales."
The spokesman said the price of the vaccine to the NHS was "commercially sensitive" and was "not publicly available".
The cost of providing the immunisation programme depended on several factors, such as the eligible population size and anticipated uptake levels, he added.
- Published19 July 2017

- Published21 December 2015

- Published14 July 2015
